Anxiety
Rumination, Worry and the Brain
Research indicates a potential biomarker for depressive rumination.
Posted August 28, 2023 Reviewed by Tyler Woods
Key points
- Rumination (a focus on events in the past) can make us more susceptible to depression.
- Activity patterns in the default mode network may serve as a biomarker for depressive rumination.
- The hope is that research like this might help clinicians develop new strategies to depression and more.

Change can be difficult to deal with, and the bigger the change, the more difficult the struggle to adapt to that change can be. When we look back on what happened in the past, we often engage in what psychologists call counterfactual thinking. Counterfactual thinking happens when we generate alternatives to reality. If we imagine an alternative to reality that is better than what actually happened, we’re engaging in upward counterfactual thinking. The opposite kind of counterfactual, creating what is called a downward counterfactual, involves imagining an alternative reality that is worse than what actually happened (Epstude and Roese, 2008).
We all use counterfactual thinking on a regular basis. This kind of cognition helps us regulate our emotions and our behavior. However, focusing all of our cognitive energy on what might have been is not particularly helpful. Repetitively and passively focusing on negative events in the past is called rumination (Smith and Alloy, 2009). We tend to ruminate when we’re sad, or when we’re concerned that we’ve made a big mistake, as well as when we might actually be depressed. It is the repetitiveness of rumination, the difficulty in turning it off, that can lead to trouble. It can keep us mired in the past, looking backward instead of forward, and may make us more vulnerable to depression.
Thinking in the other direction, focusing on events in the future that might have a negative outcome but that have not yet happened is worry. Times of uncertainty, in general, can lead us to worry. When things are uncertain, there is actually more to worry about—finances, mortgages, relationships with others, and our health, just to name a few. We often worry about what might happen next to try to avoid negative consequences or to try to gain some control over events to come. However, just as with constant rumination, worrying without end, engaging in worry without being able to turn it off, can make adjusting to any kind of change more difficult.
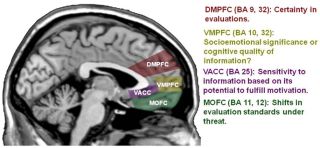
Research has linked both rumination and worry to changes in brain function, in particular, to changes in function in those all-important frontal lobes. For example, Martin, Ressler, Binder, and Nemeroff (2009) reviewed the work done on the effects of anxiety (frequently a by-product of both worry and rumination) to changes in the balance between emotional centers in the brain (like the limbic system, in particular the hippocampus and amygdala) and regions involved in higher cognition like the prefrontal cortex (PFC), which regulates executive functions like planning, decision-making, and predicting the consequences of our behaviors, and the orbitofrontal cortex (OFC), which is involved in memory, impulse control and mood. Drugs that act as effective anxiolytics and antidepressants affect neurotransmitters used by these regions of the brain as they reduce anxiety and depression.
In a recent study focused on rumination, Kim, et al., (2023) examined the effects of rumination on the default mode network. One focus of their research was to develop a way to predict rumination that might lead to vulnerability to depression. They used resting-state fMRI scans (rsfMRI). In a rsfMRI scan, images of brain function are taken when we’re not working on any particular task, when we are, as the name suggests, just resting. These scans provide researchers with a view of how brain regions work together in networks when we’re not actively trying to problem solve and can highlight individual differences in the spontaneous functioning of the brain across individuals (see Lee, Smyser, and Shimony, 2013, for a review).
In the Kim, et al. study, participants were given the Ruminative Response Scale (RSS) to assess how much and how often participants engaged in repetitive and persistent rumination, along with a variety of paper and pencil measures of both depression and anxiety. During rsfMRI scanning, participants were asked to stare at a fixation spot while in the scanner and to let their thoughts flow naturally.
.png.jpg?itok=70LedcTB)
Their results showed that activation of the default-mode network was linked to rumination. One advantage of using rsfMRI scans is that researchers could create “virtual” lesions in the brain, mathematically removing parts of the system activated during the scan to see how that removal affected the pattern of activity linked to rumination. The researchers were able to identify patterns in the activation of the default mode network that predicted both rumination and depression. A total of 21 brain regions were linked to depressive rumination, including the dorsomedial PFC, the inferior temporal lobe, and the cerebellum.
The hope is that research like this might allow a better understanding of how the brain and the networks of interconnected regions within it might increase or decrease rumination and eventually help clinicians develop new strategies to treat depression and anxiety.
References
Epstude, K., and Roese, N.J. (2008). The functional theory of counterfactual thinking. Personality and Social Psychology Review. 12(2), 168-192.
Kim, J., Andrews-Hanna, J.R., Eisenbarth, H., Lux, B.K., Kim, H.J., Lee, E., Lindquist8, M.A. Losin, E.A.R., Wager, T.D., and Woo, C-W. (2023). A dorsomedial prefrontal cortex-based dynamic functional connectivity model of rumination, Nature Communications, 14, 3540, https://doi.org/10.1038/s41467-023-39142-9
Lee, M.H., Smyser, C.D., and Shimony, J.S. (2013). Resting-State fMRI: A Review of Methods and Clinical Applications, American Journal of Neuroradiology, 34, 1866-1872.
Martin, E.I., Ressler, K.J., Binder, E., and Nemeroff, C.B. (2009). The neurobiology of anxiety disorders: Brain imaging, genetics and psychoneuroendocrinology. Psychiatric Clinics of North American, 32(3), 549-575. doi:10.1016/j.psc.2009.05.004


