Health
The Role of the Gut-Brain Axis in Parkinson's Disease
Maintaining a healthy microbiome is a preventative measure.
Posted August 19, 2022 Reviewed by Hara Estroff Marano
Key points
- Parkinson's disease patients consistently demonstrate altered gut microbiome makeup.
- Gut complications such as constipation can precede the symptoms of PD by many years.
- Simple nutritional interventions can play a role in the prevention and mitigation of PD.
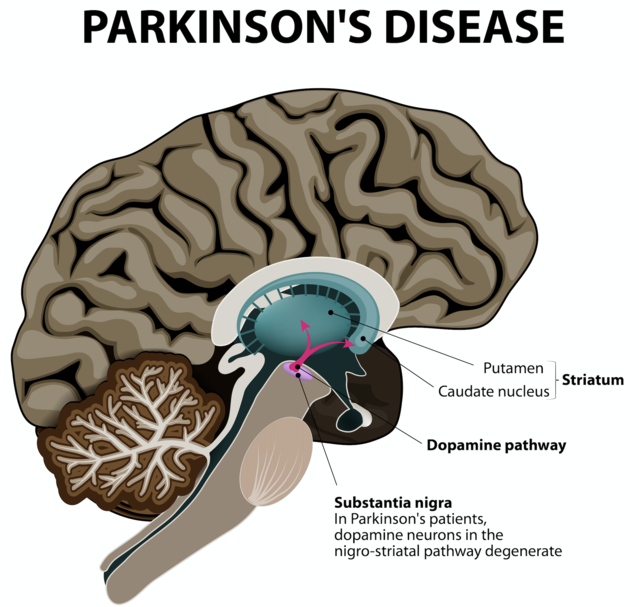
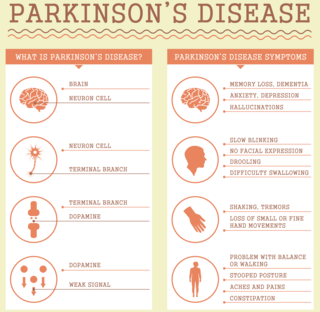
As the second-most-prevalent neurodegenerative disorder, Parkinson’s disease (PD) is expected to double in prevalence by the year 2030.1 PD development is associated with decreased dopamine levels in the brain. This “feel good” neurotransmitter is also involved in motor control, including voluntary and involuntary movement. In Parkinson’s disease, chronically low dopamine levels typically lead, progressively, to characteristic tremors, an altered sense of balance, loss of voluntary movements (akinesia), sleep disorders, depression, and gastrointestinal symptoms.2,3
One feature of the disorder is accumulation of the neuronal protein alpha-synuclein to form Lewy bodies, which lead to the death of dopaminergic neurons and inflammation in the brain. Such accumulation has long been considered causative.4,5
But understanding of Parkinson's disease is changing. The current view is that it is a systemic condition affecting the central, peripheral, and enteric (intestinal) nervous systems.6,7 It bears an important relationship to the gut microbiome.
The Gut-PD Connection
In 2003, investigators traced the development of Parkinson’s disease to inhaled or ingested pathogens.8 The infectious agents, researchers found, led to the development of α-synuclein Lewy bodies, which were later shown to spread through the enteric nervous system and into the central nervous system and brain through the vagus nerve.8,9
In addition, infection in the intestines with pathogens such as the ulcer-associated H. pylori has been linked to PD-like symptoms and an increased risk of PD diagnosis.10,11 These and other findings indicate that disruption in the microbial makeup of the gut microbiome, or dysbiosis, may trigger Lewy body formation and increase the likelihood of developing Parkinson’s disease.7
Parkinson’s patients have consistently demonstrated an altered gut microbiome population compared with healthy controls.12 Although there is microbiome variation among PD patients,13-16 preclinical studies implicate a general reduction of healthy gut microbe metabolites (notably short chain fatty acids, SCFA). The dearth of SCFA is directly correlated with low-grade, system-wide inflammation, set off by the brain’s resident immune cells, the microglia, scavenging for foreign proteins such as the Lewy bodies. The activated microglia are positively correlated with the development of alpha-synuclein abnormalities:17,18 an important factor in PD development.19
GI Symptoms as an Early Indicator of PD
Constipation is extremely common in the PD population, affecting as many as 80% of patients–often preceding motor symptoms by years.20 Constipation is not the only GI tract concern for Parkinson patients, however, as excess saliva production, difficulty swallowing, indigestion, and abdominal pain are common.21
The Importance of a Balanced Gut Microbiome
Because gut dysbiosis is considered a contributing factor to both the onset and severity of PD,22 maintaining good gut health becomes a compelling preventative and mitigating tool. Fortunately, there are a few simple nutrition-focused steps that can be taken to support good gut health and well-balanced microbiome diversity.
Feed the Good Bugs
A colorful, whole-food–based diet, rich in a variety of vegetables, legumes, whole grains, and fermented foods represents an ideal food supply for healthy gut bacteria. It provides the complex carbohydrates (fibers) and nutrients they need to thrive. In turn, the fiber-favoring microbes produce the short chain fatty acids that support the strength and integrity of the intestinal barrier. A high-quality prebiotic formulation, containing fiber, can also provide nutritional support for the gut microbiome and gut-brain axis health.
Support Gut Microbial Diversity
A quality probiotic24 formulated with metabolically active strains and demonstrated to support gut health can be key. Quality probiotic formulations list the individual constituent strains used (Genus species strain), which allows for easy identification of any related research. For example, studies demonstrate a number of healthful mechanisms associated with specific strains:
- Increased short chain fatty acid production: L. casei W56, L. acidophilus W22, L. paracasei W20, L. salivarius W24, L. plantarum W62, Lc. lactis W19, B. lactis W51/W52, and B. bifidum W2325
- Strengthened intestinal barrier: B. bifidum W23, L. acidophilus W37, L. brevis W6326
- Reduced bacterial toxin load and pathogen colonization: Lc. lactis W19, B. bifidum W23, L. acidophilus W3726
Evidence of clinical efficacy of any formulation is ideal, demonstrated in human clinical studies on the final probiotic mix. Reports of clinical efficacy assure the exact combination of strains and the quality of the manufacturing process.
Final Thoughts
Neurodegenerative diseases like Parkinson’s are not only life-altering but on the rise. Current understanding that gut health plays a role in such conditions provides a unique opportunity for prevention: incorporating simple nutritional approaches to support optimal microbiome function and a healthy gut-brain connection.
References
1. Elbaz, A., Carcaillon, L., Kab, S. & Moisan, F. Epidemiology of Parkinson’s disease. Rev. Neurol. 172, 14–26 (2016).
2. Shulman, J. M., De Jager, P. L. & Feany, M. B. Parkinson’s disease: genetics and pathogenesis. Annu. Rev. Pathol. Mech. Dis. 6, 193–222 (2011).
3. Kalia, L. V., and Lang, A. E. (2015). Parkinson’s disease. Lancet 386, 896–912. doi: 10.1016/S0140-6736(14)61393-3
4. Keshavarzian, A., Engen, P., Bonvegna, S. & Cilia, R. The gut microbiome in Par- kinson’s disease: a culprit or a bystander? In Progress in Brain Research (eds Björklund, A. & Angela Cenci, M.) Vol. 252, 357–450 (Elsevier, 2020)
5. Abeliovich, A., and Gitler, A. D. (2016). Defects in trafficking bridge Parkinson’s disease pathology and genetics. Nature 539, 207–216. doi: 10.1038/nature20414
6. Romano, S., Savva, G.M., Bedarf, J.R. et al. Meta-analysis of the Parkinson’s disease gut microbiome suggests alterations linked to intestinal inflammation. npj Parkinsons Dis. 7, 27 (2021).
7. Shen T, Yue Y, He T, Huang C, Qu B, Lv W, Lai HY. The Association Between the Gut Microbiota and Parkinson's Disease, a Meta-Analysis. Front Aging Neurosci. 2021 Feb 12;13:636545.
8. Braak, H., Del Tredici, K., Rub, U., De Vos, R. A. I., Steur, E. N. H. J., and Braak, E. (2003). Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol. Aging 24, 197–211.
9. Rietdijk, C. D., Perez-Pardo, P., Garssen, J., Van Wezel, R. J., and Kraneveld, A. D. (2017). Exploring braak’s hypothesis of Parkinson’s disease. Front. Neurol. 8:37.
10. Huang, H. K., Wang, J. H., Lei, W. Y., Chen, C. L., Chang, C. Y., and Liou, L. S. (2018). Helicobacter pylori infection is associated with an increased risk of Parkinson’s disease: a population-based retrospective cohort study. Parkinsonism Relat. Disord. 47, 26–31.
11. Matheoud, D., Cannon, T., Voisin, A., Penttinen, A. M., Ramet, L., Fahmy, A. M., et al. (2019). Intestinal infection triggers Parkinson’s disease-like symptoms in Pink1(-/-) mice. Nature 571, 565–569.
12. Sampson T (2019) The impact of indigenous microbes on Parkinson’s disease. Neurobiol Dis, 104426.
13. Barichella M, Severgnini M, Cilia R, Cassani E, Bolliri C, Caronni S, Ferri V, Cancello R, Ceccarani C, Faierman S, Pinelli G, De Bellis G, Zecca L, Cereda E, Consolandi C, Pezzoli G (2019) Unraveling gut microbiota in Parkinson’s disease and atypical parkinsonism. Mov Disord 34, 396-405
14. Sun MF, Shen YQ (2018) Dysbiosis of gut microbiota and microbial metabolites in Parkinson’s disease. Ageing Res Rev 45, 53-61
15. Unger MM, Spiegel J, Dillmann K, Grundmann D, Philippeit H, Bu ̈rmann J, Faßbender K, Schwiertz A, Scha ̈fer K-H (2016) Short chain fatty acids and gut micro- biota differ between patients with Parkinson’s disease and age-matched controls. Parkinsonism Relat Disord 32, 66- 72
16. LiW,WuX,HuX,WangT,LiangS,DuanY,JinF,QinB (2017) Structural changes of gut microbiota in Parkinson’s disease and its correlation with clinical features. Sci China Life Sci 60, 1223-1233.
17. Sampson TR, Debelius JW, Thron T, Janssen S, Shastri GG, Ilhan ZE, Challis C, Schretter CE, Rocha S, Gradinaru V, Chesselet M, Keshavarzian A, Shannon KM, Krajmalnik- Brown R, Wittung-Stafshede P, Knight R, Mazmanian SK (2016) Gut microbiota regulate motor deficits and neuroin- flammation in a model of Parkinson’s disease. Cell 167, 1469-1480.e12.
18. Baizabal-Carvallo, J. F., and Alonso-Juarez, M. (2020). The link between gutdysbiosis and neuroinflammation in Parkinson’s disease. Neuroscience 432,160–173.
19. Houser MC, Tansey MG (2017) The gut-brain axis: Is intestinal inflammation a silent driver of Parkinson’s disease pathogenesis? NPJ Parkinsons Dis 3, 3.
20. Su, A., Gandhy, R., Barlow, C., and Triadafilopoulos, G. (2017). A practical review of gastrointestinal manifestations in Parkinson’s disease. Parkinsonism Relat. Disord. 39, 17–26.
21. Salat-Foix D, Suchowersky O. The management of gastrointestinal symptoms in Parkinson's disease. Expert Rev Neurother. 2012 Feb;12(2):239-48.
22. van Kessel SP, El Aidy S. Bacterial Metabolites Mirror Altered Gut Microbiota Composition in Patients with Parkinson's Disease. J Parkinsons Dis. 2019;9(s2):S359-S370. doi: 10.3233/JPD-191780. PMID: 31609701; PMCID: PMC6839483.




