Health
Cultural Sensitivity in Mental Health Care
Getting to know your audience.
Posted September 22, 2020
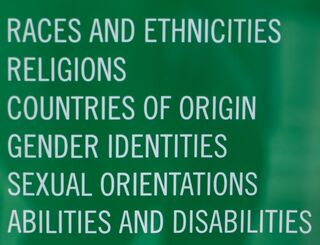
Sensitivity is a big topic. Most psychology professionals I meet are quick to have a finger on the pulse of such important considerations. While the themes of racial trauma or disparities probably come to mind, other sensitive areas such as gender identity and social class have also been much-discussed in recent years. But what about more niche cultural factors that we can encounter?
More than meets the eye
Particular nationalities and traditions can deal with life challenges or experience mental illness in vastly different ways that may appear unnecessarily challenging to providers. Instead of getting frustrated, we need to give the benefit of the doubt and realize we may not be fully understanding their experience. This should open the door to exploration with the patient and assist with forming the helping bond, central to any successful interaction. Hopefully the following four examples help readers keep this in mind:
Nothing to say
Have you ever sat with a patient who is frustratingly quiet and non-relational? On the surface, it may seem it is part of a pattern of noncompliance. I recall a court evaluation I performed on a male teenager who was of an Orthodox Jewish background. He seemed like a nice kid in presence, but was remarkably terse. This, despite the fact my evaluation would help the court understand him and likely make his life easier while dealing with the issue at hand.
Thankfully, I recalled some Jewish friends sharing that, especially in Orthodox circles, problems are your problems. It isn’t anyone else’s business, and keeping a stiff upper lip, despite the self-destruction it may encourage, is carrying on tradition and showing strength. Collaborating with a nosy mental health professional (i.e., getting personal) would violate this).
Hard to believe
Hispanic patients have more than once explained to me, “I blacked out” regarding details about some out of control experience they had. Ostensibly, this seems like an alternative to “convenient amnesia” or another excuse to not have to take responsibility. Early on I’d challenge clients who said this, or internally roll my eyes. While it would be naïve to think some aren't trying to fool us, ethnic psychopathology researchers have long known that the phenomenon is real.
The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) includes several disorders under “Cultural Concepts of Distress.” Among these is Ataque de Nervios, or Nervous Attack, unique to Hispanic populations. Symptoms include intense, acute anxiety, anger, aggression, and may include dissociative episodes like dissociative amnesia. This means the person, under immense emotional stress, experienced an alteration in consciousness that led to an inability to recall the event.
Depressingly discomforted

People working with Asian individuals may encounter patients who simply don't appear motivated for treatment. They complain of feeling handicapped by aches and pains in the absence of any obvious medical conditions. This is probably coupled with a desire to sleep a lot, and perhaps seeming inordinately lazy when awake. At first glance, you may consider writing off the patient to a physician and to come back should they be more motivated.
Intense physical symptoms always warrant a physical examination. What may surprise you, however, is that this is possibly a profoundly depressed person even though they are exhibiting all physical symptoms.
In Asian experiences, depression often manifests with significant physical symptoms (Yeung, 2006; Novick et al., 2013) and may not include the obvious sad or irritable expression that Westerner populations are used to. One possibility for this is that in a culture that substantially frowns upon lack of emotional control, it makes sense that depression is expressed as physical symptoms. These are much more acceptable than mental defect.
This is in some manner similar to Conversion Disorder (Functional Neurological Deficit Disorder) that is familiar to Western psychiatry. In Conversion Disorder, a subconscious phenomenon, people can’t, or won’t, express emotions on a conscious level, often due to potential fallout from showing emotion. That psychological energy must get discharged somehow, so is converted to physical symptoms, which are much more acceptable than mental defect. Readers interested in Conversion Disorder may enjoy Dr. Suzanne O’Sullivan’s book, Is It All In Your Head?
Double whammy
A school adjustment counselor reaches out to a black family whose child is clearly anxious and it is impacting their education. The parents acknowledge their child has struggles, but are reluctant to engage them in counseling. While a counselor might be internally screaming at the parents because it makes no sense on the surface, it is quite possible they are not simply being stubborn. One reason for balking at mental health care is the black family may feel stigma from racial discrimination, and mental illness is a compounding stigma.
What’s a helper to do?

- No jumping to conclusions. Let’s be responsive and not reactive to that terse interactional style, perceived laziness, and unwillingness to seek treatment.
- Since we’re probably truly puzzled about why someone would do such seemingly self-defeating things, let’s ask for clarification rather than calling them out on it. It is easy to be accusatory in a frustrated state: “You can make this is as easy or as difficult as you want this to be. Don’t tell me much and I’ll have to assume XYZ” and “Not engaging your kids in mental health care is irresponsible!” are not constructive offerings. Sure, tough love has its place, but right out of the gates it could give the perspective that you don’t “get them” so why should they bother?
- The most helpful thing is wanting to get to know them and showing you want to understand. Consider each of the above examples have probably encountered negative misunderstandings of their presentations, whether from parents, practitioners or society at large. If you’re not just another finger-wagger, chances are they’ll start to open up.
Setting the stage for a better interaction can begin by simply showing curiosity about their experience rather than the therapist “knowing better.” Instead of pointing out to the black family, for example, that their decision to not have their child in counselling is irresponsible, and immediately trying to convince them otherwise, inquire about previous experiences and their perspective; look out their window. After all, are we not a profession rooted in empathy?
In showing them you want to understand them you are demonstrating that interest in collaborating for the wellness of their child. Chances are, they will be more prone to hearing your concerns about the child, and open to education on mental health care, such as the possibility of referral to a culturally-appropriate counselor.
My internal eye roll or challenging “blacking out” never did much good. How could I assist in helping them deal with something I didn’t think was happening? Talking to colleagues of similar ethnicities or religious backgrounds as the person I felt frustrated with was also helpful in bolstering my empathy. Once I became curious with my clients about their experiences, our relationships improved, and we worked better.

Barring an Eye of Providence, I’ll be the first to admit there’s no perfect algorithm for fully understanding our clientele. We can, however, find ways to better interact with them about the things we don’t get, and that will benefit both parties.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Publisher.
Diego, N., Montgomery W., Aguado, J., Kadziola, Z., Xiaomei, P., Brugnoli, R., & Haro, J.M. (2013). Which Somatic symptoms are associated with an unfavorable course in Asian-Americas with major depressive disorder? Journal of Affective Disorders (149) 1-3. 182-188. https://doi.org/10.1016/j.jad.2013.01.020
Yeung, A. & Kam, R. (December 1, 2006). Recognizing and treating depression in Asian Americans. Psychiatric Times. Retrieved from https://www.psychiatrictimes.com/view/recognizing-and-treating-depressi…
O'Sullivan, Suzanne (2015). Is it all in your head? True stories of imaginary illness. Other Press, New York.




