SSRIs
Protracted Withdrawal Syndrome After Antidepressant Use
Withdrawal from widely prescribed drugs is common but mostly unstudied.
Posted January 4, 2021 Reviewed by Lybi Ma

In a 1995 issue of the American Journal of Psychiatry, amid a wave of prescribing for then-recently-approved SSRI antidepressants, physicians Lloyd Frost and Samarthji Lal wrote to warn colleagues that several of their patients complained of “shock-like sensations after discontinuation.”
A 32-year-old man they had prescribed paroxetine for an OCD diagnosis reported, two days after starting his taper, that shocks “ran quickly through his upper body and down his arms and hands.” Five months of “gradual paroxetine withdrawal” were needed to “lead to [their] cessation.”
A second patient, a 22-year-old who was prescribed sertraline, experienced the first of several similar attacks while in a swimming pool, Frost and Lal add, with a force so overwhelming he “thought he ‘was being electrocuted.’ At times his ‘whole body would fly back,’ which once led to a brief loss of control of his car’s steering wheel…. Less intense shocks persisted for 4 weeks and ceased 13 weeks after sertraline cessation.”
Although a spate of similar letters appeared in leading psychiatric journals in the mid-1990s, following the 1986 approval of fluoxetine and the 1991 and 1993 approval of sertraline and paroxetine, respectively, protracted symptoms from antidepressant withdrawal remain mostly unstudied, with official bodies on both sides of the Atlantic maintaining that SSRI and SNRI withdrawal at worst produces “transient, mild,” and self-resolving symptoms lasting up to 7-14 days after treatment.
The paucity of reliable studies even three decades later is all the more concerning because, as Michael P. Hengartner and colleagues note in the latest issue of Therapeutic Advances in Psychopharmacology, “Antidepressants are the most widely prescribed psychiatric drugs worldwide, with prescription rates ranging from about 6 percent to 16 percent in European countries and North America.” Given such percentages and the numbers of people they involve, it is all the more concerning that “severe and persistent withdrawal syndromes from antidepressants have long been neglected or minimized.”
In their corrective study, “Protracted withdrawal syndrome after stopping antidepressants,” published at the turn of the year, Hengartner and colleagues Lukas Schulthess, Anders Sorensen, and Adele Framer—respectively of Zurich University of Applied Sciences, the Nordic Cochrane Centre, and SurvivingAntidepressants.org, a peer support site focused on withdrawal from antidepressants—present the largest, most-detailed quantitative analysis to date of protracted withdrawal syndrome (PWS). “To the best of our knowledge,” they write of their 69-subject study, “the largest [previous] study specifically examining PWS comprised only seven case reports.”
First among several major findings: Antidepressants “of all types may incur protracted withdrawal potentially lasting months to many years, as has been observed for other psychotropics.” Too-long understudied and too-often misdiagnosed, PWS represents a “severe and debilitating condition, which can lead even to suicide.”
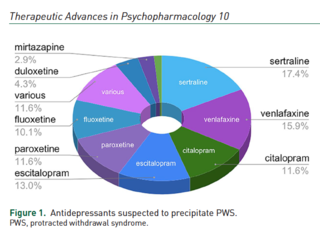
Second, six drugs—sertraline, venlafaxine, citalopram, escitalopram, paroxetine, and fluoxetine—were implicated in 80 percent of PWS cases.
Third, “comprehensive assessment of medication history, duration of withdrawal syndrome, and its various somatic, affective, sleep, and cognitive symptoms,” is needed as focusing on affective symptoms alone can lead to misdiagnosis.
Fourth, and equally important, “protracted withdrawal does not seem very amenable to reinstatement [of the drug withdrawn] or other conventional drug treatment,” raising the possibility that the condition “may be mistaken for a ‘treatment-resistant’ psychiatric condition.” As noted, “attempted by about a quarter of our study population, reinstatement was successful in fewer than half.”
The study selected 69 individual reports of protracted withdrawal for analysis, based on diagnostic criteria proposed by Chouinard and Chouinard (2015), involving at least 6 months of continuous antidepressant use. Duration of PWS ranged from 5 to 166 months, with the length of time on the antidepressant causing the withdrawal ranging from 6 to 278 months.
Of the 69 subjects, 19 “reported having gone off the drug abruptly (the rest having done some sort of taper) and 21 (30.4 percent) had withdrawal symptoms during tapering. 33 (47.8 percent) had previous but unsuccessful withdrawal attempts or other adverse drug reactions.
Throughout the withdrawal experience, affective symptoms—mostly anxiety, depression, emerging suicidality, and agitation—were reported by 81 percent. Somatic symptoms, mostly headache, fatigue, dizziness, brain zaps, visual changes, muscle aches, tremors, diarrhea, and nausea, were experienced by 75 percent. Sleep problems (44 percent) and cognitive impairments (32 percent) were mentioned less frequently.
After several weeks of flu-like symptoms, following a tapering of paroxetine, one participant wrote: “I got hit like a truck with crazy unexplainable symptoms: waves of panic that felt different from my original anxiety/panic, OCD about symptoms and thoughts, feeling disconnected from the world around me, phantom smells (always the same burning smell), insomnia, vivid and wacky dreams, horrible ringing in my ears and head (almost feels like an electric current), weird burning/shivering of my brain, and more. These were so debilitating to me I left my job and am currently unable to function.”
Another wrote of coming off citalopram: “I took 2 weeks' leave from work in anticipation of the withdrawal. At first, there were only brain zaps and some agitation that in itself was manageable, then came the gastrointestinal issues about 1 month after stopping the meds, mostly heartburn and IBS (irritable bowel syndrome) type symptoms. I did not link these issues with withdrawal and went to a GI specialist that performed multiple tests (colonoscopy, gastroscopy, CT scan, and blood tests); all tests came back reporting no issues. After about two months off the meds, I started having severe panic attacks and anxiety as well as pressure in my head (behind my eyes), severe dizziness, and a lot more symptoms that I cannot even recall as they disappeared and reappeared seemingly at random.”
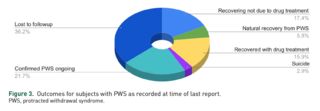
Four persons reported natural recovery from PWS without reinstatement or drug treatment; 12 reported an improvement short of full recovery. Two persons died by suicide. More than one-third of the sample was lost to follow-up, complicating outcome assessment.
In multiple Internet support groups, one of the women who had suicided repeatedly “expressed distress about her ongoing sexual dysfunction”—Post-SSRI Sexual Dysfunction (PSSD)—which had persisted, despite treatment with mianserin, for 38 months. Her last post on SurvivingAntidepressants.org was in October 2019: “To be honest, now I’m in absolute hell. I don’t see much hope in this situation anymore. It’s been 3+ years and I’m still in pretty much the same situation. I don’t know how much longer I’ll be here honestly.” The following day, she killed herself. She had recently turned 21 years old.
The second woman had endured 69 months of PWS, clearly and repeatedly expressing anguish over her iatrogenic condition before she, too, killed herself.
“As with other psychotropics,” Hengartner and colleagues warn, “the potential for antidepressant PWS is embedded in pharmaco-dynamic adaptations and possibly irreversible neurophysiological alterations following prolonged drug exposure.” Consequently, they are especially concerned that their findings reach general practitioners (GPs) and mental health professionals to ensure better recognition of the condition and least harmful ways of treating it. Given the neurophysiological adjustments involved, slow and gradual tapering by microdosage over months is always preferable to an abrupt termination.
Acknowledging the limitations to their study, including its modest-sized sample and data “derived from spontaneous self-reports,” Hengartner and colleagues urge that large prospective cohort studies and clinical trials try to “replicate our exploratory findings and … further examine associations between patient characteristics, medication histories, antidepressant drugs and classes, duration of treatment, and the varying manifestations of protracted antidepressant withdrawal.”
“To me,” Hengartner replied to a follow-up question about longer-term implications, “the main message of our study is that protracted withdrawal from antidepressants presents in various manifestations, with multiple waxing and waning symptoms, both mental and physical. You can’t pin it down to one or two core symptoms. It’s a very complex, multifactorial syndrome. What’s also a very important message is that in some cases it spontaneously improves, even after many months. Sadly, in some cases, the syndrome persists for many years and doesn’t seem amenable to treatment. But there is hope that the symptoms will eventually resolve when the body readapts.”
Framer emphasized the suffering behind the data: “I hope readers of this paper sense the heartbreak behind these statistics. Protracted withdrawal syndromes destroy lives. SurvivingAntidepressants.org is only one node in the vast online peer support network for psychiatric drug withdrawal, which sees thousands of ongoing human tragedies every day. The ignored or unexamined risks of psychiatric drugs are not theoretical; they cause real harm. Medicine should be doing everything it can to prevent these adverse outcomes.”
References
Chouinard, G, and Chouinard, VA. 2015. New classification of selective serotonin reuptake inhibitor withdrawal. Psychother Psychosom, 84: 63–71. [Link]
Hengartner, MP, Schulthess, L, Sorensen, A, and Framer, A. (12.24.2020). Protracted withdrawal syndrome after stopping antidepressants: a descriptive quantitative analysis of consumer narratives from a large internet forum. Therapeutic Advances in Psychopharmacology, 10: 1–13. https://doi.org/10.1177/2045125320980573 [Link]




