
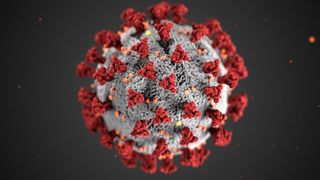
Coronavirus Disease 2019
Coronavirus: The Importance of Viral Load
Recognizing viral dose may lead to less and less severe infections.
Posted April 3, 2020 Reviewed by Gary Drevitch
Who gets sick? Much of COVID-19’s prevalence, severity, and lethality may have to do with viral particles you are exposed to—the issue of viral load, also called viral dose.
Not much is written on this subject because it is difficult to study, but we can learn a little from studies on flu. In one frequently cited article, patients with flu put out 900 to over 300,000 viral particles per cough, less than when they were feeling OK, though still appreciable amounts (averaging 75,000 particles per cough when ill, 52,000 when not). People do not realize that when they’re having a conversation they are spitting out particles, including viruses, in very large amounts, mostly because we don’t see them. (To have an idea of how microdroplets spread and stick around, watch this video). In the same flu study, about 63% of the particles expelled were the right size to embed in the lung. Other studies argue that viral particles are expelled even more effectively by talking.
Coronavirus will be different from flu, but the principle is the same: talking, singing, praying, kissing, nuzzling, all produce lots of coronavirus particles. Much of the reporting on coronavirus seems to make people think infection is a quantum, complete effect like neural transmission: if a single virus particle embeds in my nasopharynx, I’m done.
No. If you are sitting praying in a church or synagogue next to hundreds of others, or at a close-set dinner party, or a psychotherapy session in a small closed room, chances are better you will be exposed to the several hundred viral particles presently postulated as needed to cause general infection.
Fortunately, what’s called our innate immune system prevents us from getting heavily infected, and if infected, ill. Otherwise, you and I would not be here.
Now, consider the plight of health care workers in Wuhan and northern Italy. Even with the best of protective equipment in the foremost teaching hospitals, you are surrounded by sick people who are expelling lots of virus particles. With "perfect" technique, you may still infect other hospitalized patients as well as your colleagues. Globally doctors plead with governments about the lack of personal protective equipment required to fight the virus effectively. The end result is sick health care workers infecting patients and each other, with higher mortality. Overall, the people who are getting sick most frequently and most ferociously are family members (75-80% of cases in Wuhan), friends, and co-workers, depending on their individual immune response (see below).
Bottom line: Social distancing is critical. You can understand the importance of social distancing if you visualize yourself and others spewing out viral particles as you speak. It’s also known that a larger viral load leads to more, and sicker, flu cases. Will that happen with COVID-19? Many think so, but convincing data will be hard to obtain.
The two lessons of viral load: social distancing works, and we may well benefit from the general use of masks.
A paper from the southern Netherlands (not yet peer-reviewed) demonstrates just how remarkably prevalent COVID-19 might be throughout the world.
In a cross-sectional study, health care workers at two teaching hospitals were asked whether they recently had fever or mild respiratory symptoms. This was done just two weeks after the first case in the country was diagnosed, on February 27. A very high 14% reported symptoms, and were tested for the presence of virus in their nasopharynx.
In that group, 6.4% tested positive. Of this group shown to carry COVID-19, a little over half reported fevers. Nearly two-thirds of them kept working. Importantly, 8% reported feeling sick even before the first Dutch COVID-19 case was diagnosed.
Most interesting, only 3.5% had exposure to a known COVID-19 patient. The authors concluded that a sizable part of the population had already been infected with COVID-19 before patients began appearing in any Dutch hospital.
Take a look at the numbers. If you assume that all of the hospital workers who were asymptomatic were not infected, which is probably dead wrong, you had about 1% of healthcare workers infected with COVID-19 only two weeks after the first diagnosed case in the country. The people of the town of Vo in northern Italy showed 3% were infected very early in the virus's spread.
Bottom line: Just as Chancellor Merkel said weeks ago that 60-70% of the German population might eventually be infected, COVID-19 is going through the population rapidly, with many of those infected having no idea. It’s important to recognize that infection does not equal illness.
What is necessary now is testing, both for infection—the appearance of the virus in the nasopharynx, where even asymptomatic folks can infect others, and of serology, whether people have mounted an antibody response.
There are already numerous prototype machines that should be able to do such testing in less than an hour. We need those machines verified by independent labs. Then we can send out field epidemiology teams to work with local health departments across the nation to find out who is infected, and who has an antibody response. That information will be very useful in helping decrease the infection and plan our public health and economic future. Which brings up the issue of immunity.
Individual immunity varies a lot, as does population immunity. The level of mortality may in part by viral load. It’s just one of many factors that might help explain why the mortality rate in Germany has so far been lower than that in Italy and Spain.
Immunity is robust when a population is healthy. One lesson people should learn is the health of every person affects their health, and your health affects everybody else’s. Potentates should recognize that if the homeless get infected, so can they.
Still individual immunity varies vastly from one person to another. Some may be highly susceptible to coronavirus while others are not, due to quirks of their genetics, medical and personal history. Some doctors will move through patient after patient in the ICU and never get sick, while citizens who never meet an “ill” person develop a lethal infection.
So you want to do what you can to keep your individual immunity as effective as you can.
Bottom line: The public health is your health. To maintain your own immunity:
- Socially distance. The less of a viral load you are exposed to, the less risk of infection and illness. Hopefully, a 6-foot distance is enough to keep the viral particles we normally expel from infecting others. Masks should help.
- Walk. People get fewer colds and less severe ones when they move; the studies were in open environments, but moving indoors is still exercise.
- Sunlight is a drug that enhances immunity and mood, and works well through your eyes; you don't want to look at the sun, as reflected light works. Perhaps increased vitamin D from skin exposure may also help immunity.
- Eat. Illness and stress cause can cause more metabolic breakdown, requiring better than usual nutrition. Get real, whole foods, not just comfort foods, as varied as you can.
- Sleep. Immunity to colds is known to be much worse when people are sleep-deprived—another reason why medical personnel are very much at risk of viral infection and illness.
This is a global pandemic, but there’s plenty you do can as an individual to make it less likely you and others will get sick. One of those actions is to convince all you know they can spread infection unknowingly, just with their breath. Conversation carries risk.



