Diet
How Does Metabolic Rate Really Change After Anorexia? Part 2
Science of metabolic changes in anorexia recovery: Minnesota Starvation Study
Posted March 31, 2016
By the end of my last post, I’d concluded some basic things about metabolic rate and recovery from the contemporary science of eating-disorder research. Firstly, basal metabolic rate (BMR) and resting energy expenditure (REE) (not quite the same, but similar) decrease in the long-term undereating characteristic of anorexia. Secondly, BMR/REE increases again during refeeding, perhaps to above-normal levels. And thirdly, by the time someone is fully recovered, their metabolic rate will probably be back completely to normal.
Existing studies don’t, however, tell us much about the metabolic changes that happen in the later stages of weight restoration, after we pass beyond the bare-minimum ‘healthy’ BMIs at which clinical studies tend to stop. Insight into what carries on changing in this phase is important if we’re to dare to bring full recovery within reach by eating beyond the bodyweight anorexia calls just-about acceptable, and out into the life beyond, no longer balanced on the tyrannically precarious threshold between too little and too much.
To find out about later recovery – the phase that takes us from 'recovering' to 'truly well again' – we have to turn back the clock 70 years, to the famous ‘Minnesota Starvation Study’ (carried out by Ancel Keys and his colleagues in 1944-45, and published in 1950), which dared to do what no contemporary study seems willing to: allow its participants to get actually better. (The experimenters were also able to do what no one today would get ethical permission for: starve their participants before refeeding them – somewhat ironically, given how many people would probably volunteer for it these days.) This was, we must remember, a study not of anorexia, but of human starvation more broadly, and unlike virtually all anorexia studies, the participants were men not women. But when it comes to the physiology of starvation, there is still no fuller exploration. And when it comes to metabolic rate in particular, sex probably makes little difference: adjusted for body composition, resting metabolic rate is probably about the same in men and women (Buchholz et al., 2001). I’ve written a bit about the study here, from the perspective of how seriously we need to take the physical side of recovery as inseparable from the psychological. The two fat volumes reporting the background, methods, and results of the study, which I took out of the library a few weeks ago to explore more thoroughly than I had before, are fascinating reading, and a source of information that remains irreplaceable. I wish the full text were available online somewhere so its insights could be more easily shared.
36 healthy young men (conscientious objectors) volunteered for the study to help the Allied post-war aid effort for those suffering from malnutrition. After a 12-week control period, the volunteers were allocated a semi-starvation diet adjusted for individual metabolic needs and nutritional status, to induce the same degree of starvation in all participants, with target weight loss being an average of 24% of initial bodyweight. The men were fed an average of 1,750 kcal a day, consisting of two meals of three basic menus repeated in rotation, with lots of bread, potato, cereals, turnip, and cabbage, and only ‘token amounts’ of meat and dairy products (p. 74), to replicate conditions in European famine areas. Small adjustments were made as needed to keep weight loss close to a predicted curve, and a buddy system was introduced so that when participants left the lab they weren’t tempted to eat more than planned. A strenuous programme of physical activity (including a few hours a day of varied work and maintenance tasks, plus about 6 hours’ walking a day) was strictly maintained throughout, with free time only in the evenings and on Sundays. During the 24 weeks of semi-starvation, the rate of change in BMR was proportional to the rate of weight loss, resulting in a total average reduction of 40% per man, or 30% per square metre of body surface, or 20% per kg, or 15.5% per unit of active tissue (pp. 328-329). That is, as observed in the other studies I’ve discussed, the metabolic change doesn’t just reflect the loss in active tissue, but represents a significant reduction beyond that.
After the semi-starvation phase, participants were split into four groups (with energy needs roughly balanced across the groups), and the plan was to give them an estimated supplement – over their daily minimum energy balance requirement – of 400, 800, 1,200, and 1,600 kcal respectively (though subsequent calculations revealed that the true amount given may have been slightly lower). But the plan turned out to be impractical:
At the end of the sixth week of rehabilitation it became apparent that only a very small degree of rehabilitation was being achieved in the subjects comprising the 2 lower caloric groups. The subjects were becoming discouraged and problems of morale were arising. Consequently, with the start of the seventh week of rehabilitation, the intake of all 4 caloric groups was increased by an average of about 800 Cal. (p. 77)
[T]he expected ‘new lease of life’ did not materialize. […] Hunger and appetite were not appeased. As one subject expressed it, ‘Now I go away from meals hungry three times a day instead of two.’ Some men reported that their hunger pangs seemed more intense than ever before. […] Some of them became more depressed and irritable than in semi-starvation. […] Impatience, tenseness, and a feeling of being ‘let down’ pervaded the group. (p. 838)
Another increase of on average 259 kcal/day was then made after week 10 of rehabilitation. If read through the lens of anorexia recovery, this is pretty striking: even with an increase of 1,600 kcal/day, which is probably about three times what most people in outpatient recovery attempt to begin with, weight gain was too slow to be physically or psychologically viable. It’s strange imagining anything like this being reported in an anorexia study: the patients lost morale and wanted more to eat. Though many of the men’s psychological states came to look very much like anorexia, their responses to the rehabilitation phase give us a telling sense of what recovery from starvation looks like without the anorexic drive for thinness or control or self-negation: the men just wanted the hunger to be over. Thus it provides a wonderfully reassuring model for how recovery could be if we let it.
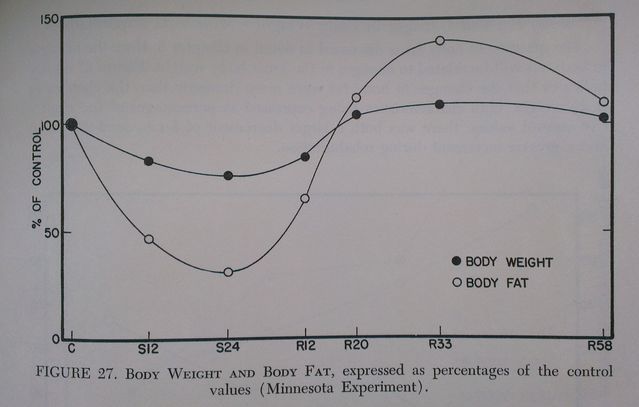
Structured rehabilitation lasted for 12 weeks, after which 12 participants volunteered to remain at the lab for a further 8 weeks, during which time they were allowed to eat as much as they wanted. Further follow-up tests were carried out on some participants at weeks 33 and 55-58 of the rehabilitation period (R33 and R55-58). The prestarvation control bodyweight was reached by participants from all refeeding groups by R16, while by R20 it had reached around 105% of control levels, and by R55-58 it was up to 109%, with the excess accounted for by extra fat storage. By R58 bodyweight and bodyfat values had returned almost exactly to prestarvation levels, with total average bodyweight at 69.8 kg as opposed to the original 69.5, and bodyfat as a percentage of total weight now at 15.2% rather than 13.9% (p. 284) (see Figure 1). Although two men (neither of them amongst those monitored at the lab beyond R12) reported deliberate weight control strategies at R20 – one skipping breakfast to lose weight, the other aiming to stabilise his weight at 8 kg below his original weight – in general everyone’s eating habits and attitudes towards food were gradually normalising: less wolfing-down of meals, less preoccupation with (particularly sweet and dairy) food and fear of it being withdrawn, more interest in other things again (pp. 842-53).
As for the return of metabolic rate to normal levels – by R6 the lower-calorie groups had regained around 10% of the lost BMR, and the higher-calorie groups between 25% and 30%. At R12 the four groups had regained between 20.9% and 57.1% of their original bodyweight, and had regained between about 35% and 70% of the loss in BMR (per square metre of body surface) depending on energy intake (see Figure 2). By R20 the bodyweight of those measured had overshot the prestarvation weight by an average of between 4.6 and 2.1 kg, and the BMR of all 12 men was at slightly (a few percentage points) above prestarvation levels (p. 1159).
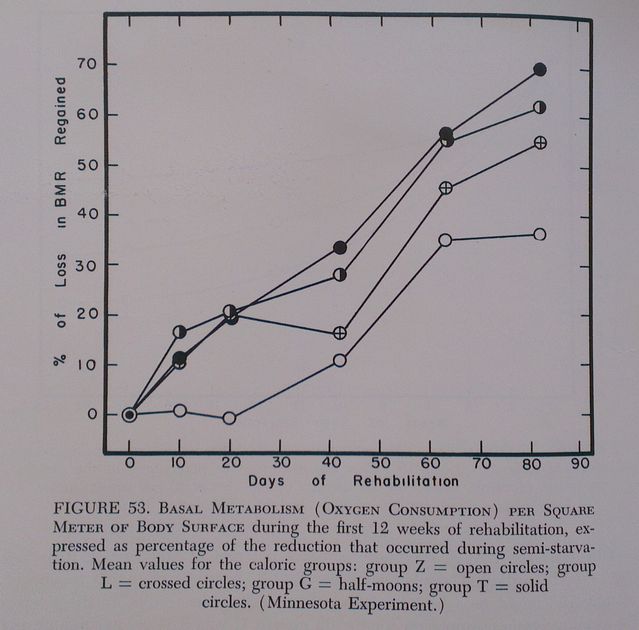
The data as presented aren’t detailed enough to establish exactly when the BMR returned to normal (and then overshot slightly), but it happened somewhere between R12 and R20, i.e. after the participants began to eat unrestrictedly again, and around the same time as bodyweight returned to its prestarvation levels too (which happened by R16). We can infer that its return to normal would have taken longer had the restricted diet (which, remember, was already significantly more generous than most anorexic recovery diets) been maintained for longer.
The simple but important upshot of all this is threefold: 1) that the longer dietary intake is restricted, the longer it will take for the metabolism as well as bodyweight to return to normal levels, 2) that a degree of bodyweight and bodyfat overshoot is normal, and reversed within around 9 to 10 months of the start of overshoot, and 3) that if you keep restricting your intake, all you’re doing is holding your body in a starvation state in which it needs less energy to maintain a given weight, by reducing ‘nonessential’ functions in a way that significantly impairs everyday quality of life. In plain English, eating less means you need less to keep your weight at a given level. Eating more means your body will use more energy for other important things.
The reasons for the overshoot in bodyweight may be partially physiological, as I set out in my previous post, and partly psychological. Keys and colleagues speculate as follows about the mental difficulties the men experienced in stopping eating after they were allowed to eat freely again:
It may be that the subjects remained more conscious of hunger pangs than they were before participating in the experiment. At any rate, they had very low resistance to eating snacks between meals. Some men reported that at times they had a physical sensation of hunger even after they had eaten a large meal; subject No. 27 commented at the end of R13 on having “an odd sensation of being full yet still hungry.” On the personality level there was anxiety, only rarely verbalized, that the food somehow would not last. For example, subject No. 29 decreased his intake only at R21 when he was no longer apprehensive that there would not be enough food. (p. 128)
In anorexia recovery in the 21st century, the explicit anxiety that the food won’t last may not be experienced in the same way as for volunteers during WWII, but the hunger overlain by satiety is the same, and the bodily lack of confidence in continuing availability of adequate food will be the same too. The crucial thing to bear in mind is that this is all right. For women, the overshoot in bodyfat will likely be slightly greater, since baseline levels are higher too, but the same pattern of response as shown in Figure 1 will hold true, if you let it.
So, in conclusion: with unrestricted eating, both bodyweight (and bodyfat) and metabolism will return to normal, overshoot slightly, and then drop back to normal, at around the same time. As it was for these men, starting with a regulated diet and only later relaxing that tight control into a proportionate response to continuing hunger is probably the safest thing, physically and psychologically. But that second stage should happen; it’s what tells your body that it needn’t be afraid of famine any more.
If you’re contemplating or halfway through the frightening process of regaining weight after starvation, take heart from this remarkable experiment, and the bravery of the 36 men who volunteered for it, and don’t hold your body captive in a diet that will defer your return to health for months or years beyond when it might happen – or perhaps forever. You may have become ill before you were fully grown, so that you have no clear idea of your ‘control’ weight; you may have been ill far longer than these men fasted, or have starved yourself on quite a different diet. But all the evidence we have points to the fact that your body will respond to restriction, and to its lifting, just as theirs did.
References
Buchholz, A.C., Rafii, M., and Pencharz, P.B. (2001). Is resting metabolic rate different between men and women? British Journal of Nutrition, 86(6), 641-646. Abstract here.
Keys, A., Brožek, J., Henschel, A., Mickelsen, O., and Taylor, H.L. (1950). The biology of human starvation. 2 vols. University of Minnesota Press. Amazon preview of Vol. 1 here.




