Pregnancy
Coronavirus and Pregnancy: What Are the Risks?
Effects of the pandemic on pregnancy fortunately seem to be limited.
Posted July 28, 2020
When British Prime Minister Boris Johnson was hospitalized with a coronavirus infection and spent some days in intensive care, a media flurry ensued. The virus also afflicted his pregnant fiancée Carrie Symonds, but that received far less attention, maybe reflecting laudable concern for her privacy.
Just 25 days before giving birth, Symonds herself announced on Twitter: “I've spent the past week in bed with the main symptoms of Coronavirus. I haven't needed to be tested and, after seven days of rest, I feel stronger and I'm on the mend.” Considerately, she quickly posted a follow-up tweet, linking to very useful guidelines from the Royal College of Obstetricians & Gynaecologists: “Being pregnant with Covid-19 is obviously worrying. To other pregnant women, please do read and follow the most up to date guidance which I found to be v reassuring.” This thoughtful gesture hopefully comforted many other pregnant victims of the pandemic, naturally concerned about possible side-effects. Thankfully, current evidence indicates that major complications are rare for both mothers and fetuses/babies.
Coronavirus during pregnancy
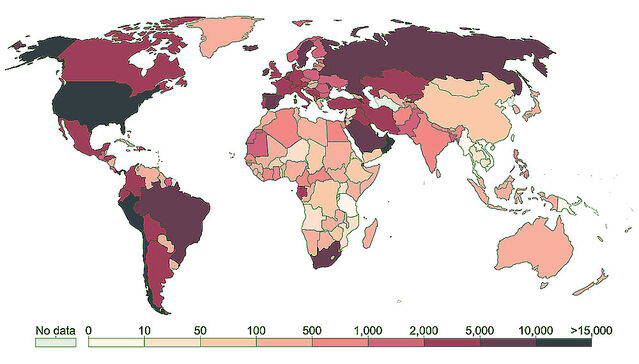
With almost 17 million cases worldwide so far, the pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has inevitably infected vast numbers of women at some stage of pregnancy. Pregnant women might be particularly susceptible to infection, and prior findings with other coronaviruses indicated adverse effects on fetal development. Earlier this year, Guillaume Favre and colleagues noted that severe acute respiratory syndrome (SARS-CoV) and Middle East respiratory syndrome (MERS-CoV) were both associated with serious complications during pregnancy—including miscarriage, fetal growth restriction and premature birth, sometimes with fatal consequences. They recommended systematic screening for coronavirus disease 2019 (COVID-19) during pregnancy.

Because the current pandemic began under nine months ago, medical evidence is scarce and largely confined to birth outcomes. Several projects have been initiated to assess impacts on pregnancies, but most are only just beginning. In addition to premature birth, potential complications include Caesarean sections and separation (abruption) of the placenta. A key question is whether the mother can transmit coronavirus across the placenta or during breastfeeding. Regarding the latter, a brand new paper by Christine Salvatore and others provides reassurance. These authors studied over a hundred mothers who tested positive for SARS-CoV-2 and were all allowed to breastfeed. With appropriate hygiene precautions—including women wearing a face-mask while breastfeeding and regularly cleansing their breasts and hands—all babies consistently yielded negative test results and none showed symptoms of infection.
The question of whether pregnant women are more susceptible to COVID-19 has already been answered as well. Noelle Breslin and colleagues reported on 43 infected pregnant women in two New York City hospitals between 13 and 27 March. Disease was mild in 37 women (86%), severe in 4 (9.3%) and critical in 2 (4.7%). These figures are close to those for non-pregnant women with coronavirus (80% mild, 15% severe, and 5% critical).
Preliminary findings with pregnant women
Drawing on experience at a hospital in Wuhan (China) where the pandemic began, Lu Zhang and colleagues reported on effects of coronavirus during pregnancy. A small sample of 18 late-term pregnant women treated for pneumonia associated with COVID-19 gave birth at 35-41 weeks of pregnancy. By definition, any birth before 37 weeks is premature, and 3 births in the Wuhan sample (17%) fell into that category. All 18 infants tested negatively for coronavirus after birth, indicating no vertical transmission from the mother. Notably, 17 infants (94%) were delivered by C-section. Previously, the C-section rate at the hospital was much lower, at 50%.
Subsequently, Valeria Savasi and others reported findings from a larger sample of 77 late-pregnant women infected by coronavirus. All were patients in 12 maternity hospitals in northern Italy, where the first major COVID-19 outbreak outside of China occurred. Only 57 women gave birth while hospitalized because 20 were still pregnant when discharged; 12% (7) gave birth prematurely, compared with the 2019 rate of 7%. At 39%, the C-section rate was also markedly higher than the 27% recorded for 2019. Nine infants required intensive care, but their mothers’ illness seemingly did not affect their wellbeing at birth. Encouragingly, not a single mother died. Savasi and colleagues found no indications that pregnant women were more likely to suffer severe coronavirus infection or a greater risk of early pregnancy loss, miscarriage, or congenital anomalies. Coronavirus test results were positive for four infants (3 born vaginally and 1 by C-section) that were possibly infected after birth. Although all newborns were breastfed, none showed respiratory symptoms.
Subsequently, Vinayak Smith and colleagues reviewed 9 reports on maternal and neonatal outcomes for some 50 pregnancies associated with COVID-19. Premature birth occurred in 64% , fetal distress in 61% and C-section in 80%, all higher than in the general population. Vertical transmission of coronavirus may have occurred in just one case. Maternal mortality was zero and only one patient needed intensive care with ventilation.
Surprise reduction in premature births
One consistent finding is that the premature birth rate is elevated in pregnant women infected by coronavirus. [Apparently fitting this pattern, Carrie Symonds’ baby was reportedly born several weeks before the due date.] However, it is unknown whether a higher proportion of premature births resulted directly from the mother’s infection or indirectly from precautionary C-sections.
Unexpectedly, two preliminary reports indicate that the premature birth rate for women generally—regardless of coronavirus infections—tumbled under lock-down conditions. One report by Roy Philip and colleagues, focussing on infants with very low birth weight (below 3.3 pounds), compared findings for January-April 2020 with data for the same 4-month period over the previous two decades (2001-2019). Whereas the historical rate for very low birth weight had been 8.2 cases per 1000 live births, a surprisingly low rate of only 2.2—a quarter of the previous level—occurred under lock-down in 2020!
In the second report, Gitte Hedermann and colleagues examined nationwide Danish data for over 30,000 live singleton infants born between March 12 and April 14 over the 6-year period 2015-2020. 58 infants were extremely premature at birth, with pregnancy durations below 28 weeks. Pregnancy durations for the coronavirus lock-down period in 2020 differed significantly from the stable rate over the previous five years, during which the extremely premature birth rate was ten times higher!
As pregnant women with COVID-19 are more likely to give birth prematurely, this unexpected reduction in pre-term births in women generally is evidently not a direct outcome of coronavirus. Instead, it seems that lock-down conditions led to this surprising outcome. Possible factors are general effects of social distancing, benefits of staying at home rather than commuting to work, or less stress during pregnancy. Importantly, this may throw light on the escalating problem of premature birth in the USA. Although medical advances permit survival of infants born increasingly early, death rates are high and survivors experience greater health problems throughout their lives. Any new perspective on prematurity permitting development of preventive strategies would surely be very welcome.

Guidelines for pregnant mothers
The Royal College of Obstetrics & Gynaecology (RCOG) guidelines mentioned in Carrie Symonds’ tweet are regularly updated. One key finding, mirroring findings in the USA, is inequality of outcomes for women belonging to ethnic minorities. This presumably reflects long-standing factors such as socioeconomic disadvantage, living and/or working in crowded conditions and employment in support occupations including health and social care. Whereas ethnic minorities represent 13% of the UK total population, they account for 55% of individuals admitted to critical care for COVID-19 and are more likely to die from it.
Other risk factors for pregnant women associated with hospital admission with COVID-19 infection include overweight (high Body Mass Index), pre-existing conditions (notably diabetes), and maternal age exceeding 35 years. Vitamin D deficiency has also been linked to Acute Respiratory Distress Syndrome, which arises with severe COVID-19 infections. In sum, the RCOG guidelines recommend regular exercise, a healthy diet, and vitamin D supplementation to reduce risks of adverse effects from coronavirus.
Available information indicates that impacts of COVID-19 on pregnancy are mercifully limited. Reporting on a UK study, Marian Knight and colleagues conclude that the data “suggest that most women do not have severe illness and that transmission of infection to infants of infected mothers … is uncommon."
References
Breslin, N. et al. (2020) COVID-19 infection among asymptomatic and symptomatic pregnant women: Two weeks of confirmed presentations to an affiliated pair of New York City hospitals. American Journal of Obstetrics & Gynecology 100118.
Favre, G., Pomar, L., Musso, D. & Baud, D. (2020) 2019-nCoV epidemic: what about pregnancies? Lancet 395(10224):e40
Hedermann, G., Hedley, P.L., Baekvad-Hansen, M., Hjalgrim, H., Rostgaard, K., Poorisrisak, P., Breindahl, M., Melbye, M., Hougaard, D., Christiansen, M. & Lausten-Thomsen, U. (2020) Changes in premature birth rates during the Danish nationwide COVID-19 lockdown: a nationwide register-based prevalence proportion study. medRciv DOI: 10.1101/2020.05.22.20109793
Knight, M., Bunch, K., Vousden, N., Morris, E., Simpson, S., Gale, C., O’Brien,P., Quigley, M., Brocklehurst, P. & Kurinczuk, J.J. (2020) Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in UK: national population based cohort study. British Medical Journal 369,m2107:1-7.
Lamouroux, A., Attie-Bitach, T., Martinovic, J, Leruez-Ville, M. & Ville, Y. (2020) Evidence for and against vertical transmission for SARS-CoV-2 (COVID-19). American Journal of Obstetrics & Gynecology. DOI: 10.1016/j.ajog.2020.04.039:
Philip, R.K., Purtill, H., Reidy, E., Daly, M., Imcha, M., McGrath, D., O'Connell, N.H. & Dunne, C.P. (2020) Reduction in preterm births during the COVID-19 lockdown in Ireland: a natural experiment allowing analysis of data from the prior two decades. medRciv DOI: 10.1101/2020.06.03.20121442
Royal College of Obstetricians and Gynaecologists (2020) Coronavirus (COVID-19) Infection in Pregnancy: Information for Healthcare Professionals, Version 10.1.
https://www.rcog.org.uk/en/guidelines-research-services/guidelines/coro…
Salvatore, C.M., Han, J.-Y., Acker, K.P., Tiwari, P., Jin, J., Brandler, M., Cangemi, C., Gordon, L., Parow, A., DiPace, J. & DeLaMora, P. (2020) Neonatal management and outcomes during the COVID-19 pandemic: an observation cohort study. Lancet Child & Adolescent Health DOI: 10.1016/S2352-4642(20)30235-2
Savasi, V.M., Parisi, F., Patanè, L., Ferrazzi, E., Frigerio, L., Pellegrino, A., Spinillo, A., Tateo, S., Ottoboni, M., Veronese, P., Petraglia, F., Vergani, P., Facchinetti, F., Spazzini, D. & Cetin, I. (2020) Clinical findings and disease severity in hospitalized pregnant women with coronavirus disease 2019 (COVID-19) Obstetrics & Gynecology DOI: 10.1097/AOG.0000000000003979.
Smith, V., Seo, D., Warty, R., Payne, O., Salih, M., Chin, K.L., Ofori-Asenso, R., Krishnan, D., da Silva Costa, F. Vollenhoven, B. & Wallace, E. (2020) Maternal and neonatal outcomes associated with COVID-19 infection: A systematic review. PLoS One 15(6),e0234187.
Vogel, G. (2020) New coronavirus leaves pregnant women with wrenching choices — but little data to guide them. Science.
https://www.sciencemag.org/news/2020/03/new-coronavirus-leaves-pregnant…
Zhang, L., Dong, L., Ming, L., Wei, M., Li, J., Hu, R. & Yang, J. (2020) Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection during late pregnancy: a report of 18 patients from Wuhan, China. BMC Pregnancy & Childbirth 20, Art. No. 394:1-7.




