Chronic Pain
How Pain Psychology Treatments Work
Five fundamental treatment goals of a pain psychologist
Posted May 26, 2019 Reviewed by Matt Huston
Only a small percentage of people living with chronic pain pursue help from a pain psychologist. On one hand, this is discouraging because pain psychology treatments have decades of scientific support for their benefits. Despite these proven benefits, however, mere thousands each year participate in pain psychology therapies among the millions struggling with chronic pain conditions.
On the other hand, it makes sense why few people think about a psychologist when considering treatment options for their chronic pain: most people believe that chronic pain is a medical condition, after all, and medical conditions require medical treatment. In the same way that it seems illogical for a person suffering from panic attacks to seek out a surgeon or a dentist, it seems equally illogical to most people with chronic pain to seek out a psychologist.
The reality is that no amount of scientific support will convince most people to try pain psychology therapies until a better explanation is provided to them for how these therapies can help. In this post, we review the five primary ways that pain psychologists help people with chronic pain.
1. Pain psychologists help people replace acute pain coping behaviors with chronic pain coping behaviors.
The most basic way that pain psychologists help is by showing people how to replace acute pain coping behaviors with chronic pain coping behaviors. All pain begins as acute pain; pain becomes chronic only when it persists past the expected length of time for healing to occur. We react instinctively to acute pain by avoiding painful activities, resting the painful area, seeking medical attention, and waiting for the pain symptoms to subside. These behaviors are both appropriate and effective… for acute pain. When the same pain becomes chronic, however, we need a new set of coping behaviors. Acute pain behaviors such as continued rest, activity avoidance and seeking medical care no longer help and often even worsen the disability associated with chronic pain. When you appreciate that managing chronic pain involves not only learning new chronic pain coping skills but also having to unlearn years of acute pain coping skills, then it makes more sense why a person might benefit from seeing a pain psychologist.
2. Pain psychologists promote the patient to the co-captain role in their pain management.
A second way that pain psychologists help chronic pain is by helping people adopt a leadership role in their treatment. During acute pain episodes, our role as the patient is typically to follow the instructions of our medical provider. The doctor is the expert and the clear leader in the treatment relationship. This model breaks down, however, with chronic pain. In the case of chronic pain, it is no longer effective for a person to simply follow the doctor’s advice and wait to get better. The patient with chronic pain must instead assume a more active role in their treatment, a role that may equal or even exceed the importance of their medical providers. For the successful treatment of chronic pain, the person must assume responsibility for making lifestyle changes, provide feedback to and make decisions with their physician, and become knowledgeable enough about their health to self-manage their symptoms effectively. A pain psychologist can help people in each of these latter roles.
3. Pain psychologists help people de-catastrophize their thinking about pain.
The third way that pain psychologists help chronic pain is by reducing what is known as catastrophic thinking. “Pain catastrophizing” refers to a tendency to interpret pain symptoms as a worst-case scenario. For example, pain catastrophizing might refer to the tendency for a person to interpret back pain symptoms as a sign that their back is broken or that a life-threatening tumor is causing their headaches. Pain catastrophizing activates our fight or flight response, produces fear and anxiety, and often leads to excessive treatment-seeking or an overreliance on pain medicines. If not addressed, pain catastrophizing can make the effects of chronic pain much worse than would otherwise be the case based only on a person’s medical status.
4. Pain psychologists help people spend more time with goals and values and less time with pain.
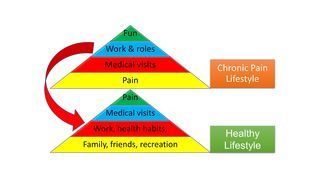
Pain psychologists also help people become less pain-focused and more value- and function-focused. Illustrated in the left image, chronic pain often takes over a person’s lifestyle, causing their days to become centered around pain, medicine-taking rituals, and medical visits. Over time, a person may become trapped in a life that has lost most sources of enjoyment, connection, and meaning. A central goal of pain psychology treatments is to help the patient resume living again in a way that is consistent with their goals and values, instead of waiting for their pain to resolve. Because chronic pain makes it difficult to be active, learning how to resume a more value- and function-oriented lifestyle is usually a process that takes time, practice, and a certain amount of trial and error.
5. Pain psychology helps decrease stress and mental health symptoms that worsen pain.
The fifth goal of a pain psychologist is to improve mental health and stress symptoms that are common to people living with chronic pain. How this part of treatment is applied varies depending on individual needs. One person, for example, may benefit from attention to pain-related depression or anxiety symptoms, whereas another person may benefit more from help to address marital or family relationships that often experience tremendous strain when someone is struggling with chronic pain.


