Post-Traumatic Stress Disorder
Is Complex PTSD a Valid Diagnosis?
Complex PTSD appears to be on the rise, but cultural changes may be responsible.
Posted April 6, 2021 Reviewed by Abigail Fagan
Key points
- The ICD-11 includes the diagnosis of CPTSD, which involves impaired emotion regulation, interpersonal difficulties, and negative self-concept after trauma.
- People most often cope and recover from trauma, but search queries for CPTSD and trauma are increasing.
- The focus on CPTSD may involve iatrogenesis—ailments caused by medical treatment, mistreatment, or misdiagnosis—and the demand for simple diagnostic labels.
Online and in real life, one encounters more and more people claiming to suffer from Complex Posttraumatic Stress Disorder — CPTSD for short. But how valid is this construct? What could explain the rise in people claiming to experience complex difficulties in recovering from trauma?
In 2020, the WHO’s International Classification of Diseases, 11th Edition (ICD11), introduced CPTSD as a new diagnostic category. Several decades in the making, the construct aimed to identify differences between classic PTSD (characterized by re-experiencing trauma, persisting avoidance, and hypervigilance) and additional symptoms of impaired emotional regulation, interpersonal difficulties, and negative self-concept.
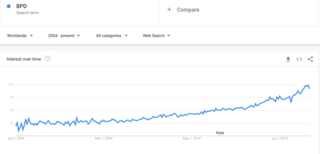
As formulations of PTSD increasingly extend to more nuanced — by some accounts increasingly vague — dimensions of daily functioning, ongoing controversies among clinicians and personality researchers point to possible comorbidities with — or confusion for — Borderline Personality Disorder. In North America, while the diagnosis may be given at some clinician’s discretion, the DSM-5 does not currently acknowledge the condition. In the meantime, the idea of CPTSD continues to gain traction in the public.
Increasing Awareness and Support for CPTSD
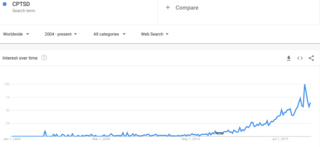
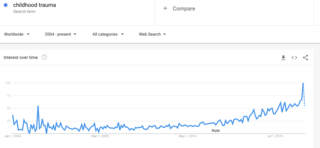
The incidence and frequency of search terms on Google, as data scientist Seth Stephens-Davidowitz demonstrated, give us a unique window into the themes of people’s fears, obsessions, and biases. These trends also show how contagious these themes can be.
Google Trends for the term “CPTSD” since 2004 show a marked, then exponential increase in worldwide searches since 2014, with a trajectory that was already well in place before the mass disruptions of the COVID-19 pandemic. While this trend could be explained by the advent of a new diagnosis, a similar spike in searches for “childhood trauma” can be observed. Google also records a steady, albeit less exponential climb for the term “BPD” (short for Borderline Personality Disorder).
The Hygiene Hypothesis may partly explain this trend. The better things get, as Moynihan’s Law projects, the worse they seem. Steady declines in crime rates and violent deaths by all causes in the US, for example, have been documented to coincide with increases in fear of crime, and a culture increasingly obsessed with safety. Decreases in infectious disease and allergen exposure in the West have similarly been shown to correlate with increases in autoimmune and allergic diseases.
From an evolutionary perspective, the normal response to trauma — or encountering a stressor — is coping and recovery. Our brain’s HPA axis is optionally designed to give us energy, and even pain-suppressing boosters during the fight or flight response.
Our cognitive and behavioural systems are similarly optimized to learn how to cope, adapt our beliefs and reflexes, and grow from stress exposure. The prolonged impaired recovery exhibited in PTSD, rather, points to rare vulnerabilities and combinations of individual and environmental factors. PTSD, complex or not, is the exception, not the norm, and more often than not reflects ongoing burden from daily stressors rather than past trauma. Could too much safety in our environments have led us to impair our resilience systems from lack of practice?
In support of this hypothesis, early projections about mass epidemics of mental illness caused by pandemic-related disruptions turned out to be wrong: rare vulnerable populations notwithstanding, the overall response seems to be one of resilience!
The Role of Iatrogenesis
Iatrogenesis is another explanation favoured by proponents of the critical psychiatry movement. Iatrogenic diseases are ailments understood to be caused by medical treatment, mistreatment, or misdiagnosis. An infamous controversy in the 1990s, for example, uncovered the role of naive therapies in accidentally implanting false memories of child abuse that led to a worsening of symptoms. The source of trauma in this case was shown to lie in the maladaptive narrative framing of experience — in plain English, picking the wrong story to make sense of, and prime one’s experiences.
While a significant body of critique rightly focuses on the unethical influence of pharmaceutical companies, or the bureaucratized pressure of insurance companies in reducing therapy to short, diagnostic-driven practice, we should note that the bulk of the demand for simple diagnostic labels likely comes from consumers themselves. People in distress simply want meaning, and what medical anthropologists call an explanatory model: they want to understand the cause of their suffering, along with expected outcomes, and avenues for healing. In our high individualistic societies where most traditional and collectives narratives, extended families, religion, and sources of support have vanished, the simplified culture of “mental health” offers a uniquely appealing solution to the burden of finding meaning.
A formal (and recall, rare) diagnosis of PTSD or CPTSD requires a lengthy process of evaluation and clinical interviews — typically with a psychiatrist, clinical psychologist, or other highly trained clinician. As a rule of thumb, one should refrain from adopting a PTSD explanatory model until one has received a formal diagnosis. More to the point, the alarming inflation (or concept creep) of the meaning of trauma in our culture deserves careful investigation. We also ought to exercise immense caution with our suggestibility to novel forms of influence that complicate simple pictures of iatrogenesis.
To this end, I offer the terms para-iatrogenic, or pseudo-iatrogenic to draw the reader’s attention to a booming alternative health cultural-industrial complex comprised of non-medical, pseudo-clinical practitioners without formal training in the diagnosis and treatment of mental disorders. Think, to name but a few, of Instagram influencers, coaches, mindfulness gurus, naturopaths, astrologers, the (unregulated) nutraceutical industry, mind-body-spirit healers, and all the neo-shamans who routinely employ folk beliefs about “mental health” to offer “trauma-informed care.”
We may now coin another term to point to a very significant vector for the spread of maladaptive explanatory models:
Istogenesis, istogenic (from the Greek istós, web): that which originates on the Internet.
For a simpler term encompassing all dimensions of my analysis (safetyist, pseudo-medical, consumer-and influencer-driven, spreading through fast media), you may simply remember the Oprah Effect, in reference to the TV star’s famous 2018 discussion of childhood trauma, which brought immense popularity to the trope of trauma-informed everything — and likely brought about untold accidental damage.
Pointing to the risk of adopting the wrong story to make sense of our distress should not be read as a full condemnation of alternative health practices. The quality time, touch, hope, and insightful techniques and insights one can gain from alternative health can certainly help one cope, heal, relax, thrive, and flourish. The point is simply to avoid locking oneself too soon, and in the wrong setting, in a diagnostic category that may do more harm than good.
Some readers may go on to receive a formal diagnosis of CPTSD. But as veteran psychiatrist and psychotherapist Irvin Yalom passionately argued, it is important to remember that humans are always much more complex, and much more interesting than the medical labels that necessarily fail to capture who they are.
While some conditions (like schizophrenia, bipolar disorder, epilepsy or drug toxicity) may have an identifiable biological dimension, diseases of the soul still elude our precise diagnostic understanding. Disordered relationships, adaptation and adjustment issues, and disordered meaning, rather, are the core dimensions of our distress. Those can only be explored — rather than quickly named — slowly, with care, courage, expert help, and an open mind.




