Post-Traumatic Stress Disorder
The Neuroscience of Post-Traumatic Stress Disorder
Neuroscientists have discovered specific brain areas linked to PTSD.
Posted November 5, 2013
Millions of Americans suffer from post-traumatic stress disorder (PTSD). What is the neuroscience behind PTSD? A new study has honed in on specific brain regions that become smaller in people with chronic PTSD. The study looked at a group of miners all exposed to the same traumatic event. Some of the miners are experiencing chronic PTSD, while others are not. What environmental and neurobiological differences make some people more prone to chronic PTSD? Could increasing brain volume in these areas prevent or alleviate PTSD?
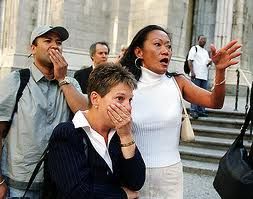
I was in lower Manhattan on September 11, 2001. It was as close to a classic PTSD inducing trauma as I’ve experienced. For millions of people, 9/11 created a lot of post-traumatic distress that lingers to this day. Luckily I didn’t develop PTSD. Have you experienced an event in your life that created post-traumatic distress? Do you suffer from PTSD? What triggers flashbacks for you? Ironically, the crystal clear September Manhattan blue sky brings back nightmarish flashbacks of the sights, sounds, and smells of September 2001 for me every year.
Who develops PTSD?
Post-traumatic stress disorder (PTSD) can develop after any terrifying experience in a person's life that causes physical or psychological harm. You don't have to be physically injured to develop PTSD. You can also develop PTSD by witnessing a friend, a family member, or even a stranger being harmed or threatened. The majority of people exposed to any type of traumatic event experience some symptoms of post-traumatic distress but most don’t develop PTSD.
One of the symptoms of people suffering from PTSD is that they become emotionally numb, and disconnected from people with whom they used to be close. This isolation often leads to substance abuse and a vicious cycle of addiction. As an educated guess, it would seem that engaging and bulking up brain regions linked to the neurobiological downward spiral of PTSD could improve outcomes.
People with chronic PTSD often lose interest in things they used to enjoy. Could this cause a downward spiral that causes certain brain areas to atrophy because they are not engaged? Most PTSD sufferers repeatedly relive the trauma and have flashbacks triggered by images, smells, sounds, or daydreams. Even decades later, someone with PTSD can have flashbacks that bring back a wave of emotions and physical sensations that mimic the intensity of when the incident originally happened, as if it was yesterday.
Is the Left superior parietal lobule the seat of PTSD?

Left superior parietal lobule.
As PTSD progresses, neuroscientists in China have recently discovered that brain structures literally change. A shrinking left superior parietal lobule was distinctly linked to PTSD. A study released in November 2013 is the first brain imaging study to identify and compare specific brain areas of individuals who had a similar traumatic exposure as connected with developing PTSD.
Understanding the brain areas linked to PTSD could be helpful in developing therapies to treat PTSD. For a three-dimensional view of the superior parietal lobule in both hemispheres please click here.
To hone in on the specific brain areas linked to PTSD, Weihui Li and colleagues from the Second Xiangya Hospital, Central South University, China compared the difference in brain structure in 12 mine disaster survivors with chronic post-traumatic stress disorder, 7 cases of improved post-traumatic stress disorder symptoms, and 14 controls who experienced the same mine disaster but did not suffer post-traumatic stress disorder, using the voxel-based morphometry method.
Their findings are published in the November 2013 issue of Neural Regeneration Research. It is interesting to note that chronic PTSD literally causes very specific regions of the left and right hemispheres of the cortex to lose brain volume. Below is a summary of their findings:
- Chronic post-traumatic stress disorder patients have gray matter structural damage in the prefrontal lobe, occipital lobe, and parietal lobe.
- After post-traumatic stress, the disorder symptoms are improved and gray matter structural damage is reduced, but did not recover to the brain volume of the control group without PTSD.
- The Left superior parietal lobule could be strongly associated with chronic PTSD.
I have written extensively in The Athlete’s Way about the importance of bulking up the gray matter of both the left and right hemispheres of the brain and creating symmetry between brain regions. One of the most interesting aspects of this new study is the imbalance seen between the brain volume in specific brain regions in the left and right hemisphere of people suffering from PTSD. By identifying specific brain areas that atrophy in people with chronic PTSD it makes sense that stimulating neurogenesis (new neuron growth) in these areas could make someone less vulnerable to post-traumatic stress disorder.
This research is in its early stages, but the results are promising. Below is a comparison of gray matter volume variations between miners with chronic PTSD, the group of miners that showed improvement, and the control group exposed to the same mining disaster that did not develop PTSD. The brain area volumes in this NRR study were measured using voxel-based morphometry analysis. Below are the specific findings of brain volume in different brain areas:
- Left superior parietal lobule (Chronic PTSD brain volume was less than control group.)
- Right superior frontal gyrus (Chronic PTSD brain volume was less than control group.)
- Right lingual gyrus (Chronic PTSD brain volume was less than PTSD group with improved symptoms.)
- Right middle occipital gyrus (PTSD group with improved symptoms brain volume was less than control group.)
- Left middle frontal gyrus (PTSD group with improved symptoms brain volume was less than control group.)
Conclusion: Balancing Brain Areas and Connectivity Could Help People with PTSD
Increasingly, neuroscientists are discovering that an imbalance—or lack of connectivity—between brain areas can be linked to mental disorders or less-than optimal brain function which take a person 'south-of-zero.' To improve mental and physical well-being, it appears that creating symmetry and connectivity between all brain areas could hold promise for taking people with PTSD, and others, 'north-of-zero.'
If you’d like to read more on this topic please check out my recent Psychology Today blogs: "Video Gaming Can Increase Brain Size and Connectivity", "Brain Asymmetry Changes a Dog's Wag and a Human's Mind", "Einstein's Genius Linked to Well-Connected Brain Hemispheres" and "The Neurobiology of Grace Under Pressure."




