Ketogenic Diet
New Study: Serious Mental Illness Improves on Ketogenic Diet
Psychiatrist in France sees unprecedented improvements in hospitalized patients.
Posted July 19, 2022 Reviewed by Kaja Perina
Key points
- Patients with major depression, bipolar disorder, and schizophrenia improved substantially on a ketogenic diet.
- The ketogenic diet was found to be safe, well tolerated by most patients, and feasible to administer in a hospital setting.
- Body weight, blood pressure, blood glucose, triglycerides, and liver enzymes improved considerably on a ketogenic diet.
- Sixty-four percent of patients were discharged from the hospital on less psychiatric medication.
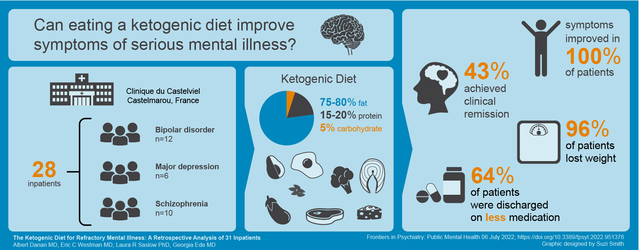
A small study conducted by University of Toulouse psychiatrist Dr. Albert Danan found that a whole-foods ketogenic diet was safe, feasible, and associated with unprecedented improvements in mental and physical health in hospitalized patients with serious mental illness.
The Inspiration for this Study
Dr. Danan is a psychiatrist practicing in Toulouse, France. The population he serves is comprised primarily of people of French and North African descent with serious, persistent mental illness, many of whom also suffer from metabolic illnesses such as obesity, hypertension, and type two diabetes.
After witnessing marked improvement in seizures and autism behaviors in a family member within several weeks of having adopted a ketogenic diet, Dr. Danan became interested in the potential of the diet to improve the psychiatric and metabolic status of his most treatment-resistant patients, regardless of diagnosis. He created a metabolic psychiatry treatment program within his local hospital where patients with chronic mental illness who had exhausted standard psychiatric therapies could attempt a ketogenic diet in a supportive, medically supervised environment.
Ketogenic Diet Protocol
Dr. Danan admitted 31 of his patients with major depression, bipolar disorder, or schizophrenia to the Clinique du Castelviel in Toulouse where they were served a ketogenic diet in lieu of standard hospital fare. The program he implemented limits total carbohydrate intake to a maximum of 20 grams per day, and was based on the ketogenic diet protocol used by Dr. Eric Westman in his metabolic research at Duke University. [A description of the diet is included in the Supplemental Data.]
Results
Symptoms of depression and psychosis improved in all 28 patients who followed the diet for longer than two weeks, with improvements becoming noticeable within three weeks or less. 43% of patients achieved clinical remission, and 64% were discharged from the hospital on less psychiatric medication. Dr. Danan had never witnessed this degree of improvement before in any of these patients—most of whom he had worked with for years or even decades, and all of whom had previously been hospitalized under his care one or more times.
Patients also experienced significant improvements in markers of metabolic health, including blood pressure, blood glucose, triglycerides, and weight:
All but one patient lost weight including 96% of those who were taking antipsychotics, and nearly half achieved clinically significant weight loss [defined as ≥5% reduction in body weight]. This welcome outcome alone makes a compelling case for the implementation of the KD [ketogenic diet] in people who are taking antipsychotic medications, whether or not psychiatric symptoms improve in response to the KD, as counteracting antipsychotic-induced weight gain is extremely difficult.
Significance
Until now, the evidence in support of ketogenic diets specifically for psychiatric conditions has been limited to hypothesis papers, animal studies, and a small but growing number of individual case reports.
As this was not a controlled trial, the extent to which the ketogenic diet may or may not have directly contributed to the outcomes reported cannot be ascertained. However, since this is the first time that a group of patients this large and this diagnostically diverse has ever been treated with a ketogenic diet in a hospital setting, these clinical observations serve to bridge the gap between existing case reports and the controlled clinical trials already underway at other institutions around the world.
When asked to reflect on his experience as principal investigator of this study, Dr. Danan said:
During my career, I’ve been struck by the limits of conventional therapies in psychiatry. Most patients relapse and have a poor quality of life. Most of them suffer from dramatic weight gain, obesity, diabetes, hypertension, and metabolic syndrome. Loss of life expectancy in this population can be measured in decades. This is a matter of public health and much more attention must be paid to these problems.
Introducing nutritional measures, particularly the ketogenic diet, helped me considerably to improve the results of therapy. Patients began improving their metabolic status by losing weight, improving blood pressure, etc., but most importantly, I observed real improvements in their psychiatric symptoms such as hallucinations, delusions, and mood instability.
After having led this study I’m convinced that nutritional measures can have a profound impact and lead to very important benefits, which makes me say that this represents the future direction to develop in psychiatric care.
Author Contributions
Albert Danan MD conceived of and implemented the intervention and generated clinical data and observations. Georgia Ede MD conducted the literature review and wrote the manuscript. Eric C. Westman MD and Laura R. Saslow PhD performed statistical analyses. All authors contributed to the article and approved the final manuscript.
References
Danan A, Westman EC, Saslow LR, Ede G. The Ketogenic Diet for Refractory Mental Illness: A Retrospective Analysis of 31 Inpatients. Frontiers in Psychiatry, 06 July 2022. https://doi.org/10.3389/fpsyt.2022.951376


