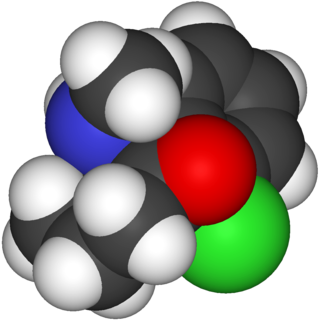
Ketamine
Ketamine Combats Depression via Unique Molecular Mechanisms
The “on/off” switch that unlocks ketamine’s antidepressant effects.
Posted December 18, 2020 Reviewed by Gary Drevitch
A new study by Canadian researchers brings us one step closer to understanding the antidepressant effects of ketamine in sub-anesthetic doses. In mice, the researchers identified how two multi-functional protein groups called 4E-BP1 and 4E-BP2 (i.e., 4E-BPs) may facilitate rapidly-acting molecular mechanisms that are key to ketamine's ability to combat depression. These findings (Aguilar-Valles, De Gregorio, Matta-Camacho, et al., 2020) were published on December 16 in the journal Nature.
"Ketamine has been proposed to exert its antidepressant effects through its metabolite (2R,6R)-hydroxynorketamine ((2R,6R)-HNK)," the authors explain. "Here we show that 4E-BP1 and 4E-BP2 are key effectors of the antidepressant activity of ketamine and (2R,6R)-HNK, and that ketamine-induced hippocampal synaptic plasticity depends on 4E-BP2 and, to a lesser extent, 4E-BP1."
"We were expecting that 4E-BPs would only be important in excitatory cells, but surprisingly, removing 4E-BPs from inhibitory cells was sufficient to block the effect of ketamine," coauthor Jean-Claude Lacaille of the University of Montreal's Department of Neurosciences said in a news release.
Ketamine: A Brief History (1960-2020) and Background Information
Since the 1960s, ketamine (i.e., Ketalar, Ketaset) has been used by anesthesiologists and veterinarians as a rapid-acting surgical anesthetic. Over the years, ketamine a.k.a. "Special K" has also gained a negative reputation as a potentially dangerous, dissociative, and hallucinogenic club drug that puts users in a "K-hole" when taken off-label in high doses.
In the U.S., some states allow police authorities to use ketamine injections to subdue criminal suspects during apprehension; this controversial practice can result in life-threatening complications.
Since the late 1990s, researchers (Berman et al., 2000) have investigated the antidepressant effects of ketamine in clinically depressed patients. In recent years, lower therapeutic doses of ketamine (i.e., esketamine) administered via a nasal spray sold under the brand name Spravato have shown promise as a rapidly acting treatment for major depressive disorders (MDD) and treatment-resistant depression (TRD).
In March 2019, the FDA approved esketamine nasal spray as an antidepressant for TRD patients; this form of ketamine is available only at certified clinics or doctor's offices. Despite FDA approval, until now, surprisingly little has been known about the molecular mechanisms that facilitate ketamine's antidepressant effects.
As Antidepressants, Ketamine and SSRIs Work Differently
Selective serotonin reuptake inhibitors (SSRIs) such as fluoxetine—which is sold generically and under the brand names Prozac or Sarafem—generally take about 14 days to kick in, if someone responds to this treatment at all. Approximately 30% of clinically-depressed patients are resistant to the antidepressant effects of SSRIs (Rush et al., 2006).
Because ketamine is rapidly-acting and can alleviate symptoms of anxious depression within 40 minutes or a few hours, it can fill a gap for treatment-resistant patients who don't respond to SSRIs or require something fast-acting.
Ketamine's Antidepressant Effects: 4E-BPs Take Center Stage
The recent (2020) study by a multidisciplinary team of Canadian researchers affiliated with Carleton University, McGill University, and Université de Montréal investigated the effects of sub-anesthetic doses of ketamine on depressive-like behaviors in mice.
As mentioned, they found that in excitatory neurons, the antidepressant activity of ketamine appears to be mediated solely by 4E-BP2. However, in inhibitory neurons, ketamine's antidepressant effects are mediated by both 4E-BP1 and 4E-BP2.
After using genetic "knockout" techniques that allowed them to remove 4E-BPs from a mouse's brain, the researchers discovered that ketamine didn't have antidepressant effects without these proteins. Based on these findings, the researchers speculate that "4E-BPs act as a switch to turn on or off the process of protein synthesis."
"This is yet another prime example of how basic research, in this case, the control of protein synthesis, leads to major discoveries in understanding disease, and the hope of curing it," coauthor Nahum Sonenberg of McGill University's Department of Biochemistry said in a news release.
Despite the hype and lofty expectations, the authors note, "ketamine remains a less-than-perfect therapy because it can be addictive." Therefore, one goal of this research is to identify the molecular mechanisms that drive ketamine's antidepressant effects so that researchers can create better and safer antidepressants that aren't habit-forming and have fewer adverse side effects.
"Too many decisions continue to be made by a trial-and-error approach that can prolong the suffering of patients and affect their quality of life," corresponding author Argel Aguilar-Valles of Carleton University's Department of Neuroscience concluded. "Our discovery has the potential to bring us closer to find a safer alternative to ketamine, and ultimately to a personalized medicine approach, where medical treatments are tailored to the individual characteristics of each patient."
References
Argel Aguilar-Valles, Danilo De Gregorio, Edna Matta-Camacho, Mohammad J. Eslamizade, Abdessattar Khlaifia, Agnieszka Skaleka, Martha Lopez-Canul, Angelica Torres-Berrio, Sara Bermudez, Gareth M. Rurak, Stephanie Simard, Natalina Salmaso, Gabriella Gobbi, Jean-Claude Lacaille, and Nahum Sonenberg. "Antidepressant Ketamine Actions Engage Cell-Specific Translation via eIF4E." Nature (First published: December 16, 2020) DO: 10.1038/s41586-020-03047-0




