Coronavirus Disease 2019
10 Ways to Lower Cytokines (Thrive) and Survive COVID-19
Threat overwhlems our immune system. The key is to thrive regardless.
Posted May 27, 2020 Reviewed by Gary Drevitch

The problem with the COVID-19 virus is not that we catch it, but that it can kill you.
There are two ways of stopping a deadly pandemic. One is through developing immunity, either by exposure to the virus or by inoculation with a vaccine. The other is to prevent people from dying. The key is to prevent the inflammatory response from reaching a level that destroys tissues and its host’s organ systems. The graph below illustrates the problem.
Cytokines
Cytokines are small signaling proteins that transmit higher-level signals and coordinate activities between cells. Consider them as the final off and on switches. They are central to modulating the immune system and inflammatory response. There are two categories of cytokines: pro-inflammatory (Pro-I) and anti-inflammatory (Anti-I). While Pro-I’s protect us by warding off acute perils, Anti-I’s keep us safe by allowing us to regenerate, thrive, and prepare us for battle with environmental enemies.
Both are necessary for survival. However, sustained elevations of Anti-I will destroy tissues in any part of the body and give rise to chronic mental and physical disease. In acute situations, levels of Pro-I may spiral out of control and cause the failure of multiple organs. This is the cause of ARDS (adult respiratory distress syndrome), the most common cause of death from COVID-19, which impedes the lungs from providing oxygen to the blood, resulting in a high mortality rate.
One term used to describe the excessive elevation of the inflammatory cytokines is “cytokine storm.” It is unclear whether there really is a “storm” or whether the normal rise of already elevated cytokines pushes people over a critical threshold into tissue edema and destruction.
Any real or perceived threat elevates Pro-I’s. That is the desired, normal response and is usually successful in protecting you from harm. However, COVID-19 can induce a powerful reaction that can kill you. The goal of treatment, aside from defeating the virus, is to prevent the levels of pro-inflammatory cytokines from crossing that fatal point of no return.
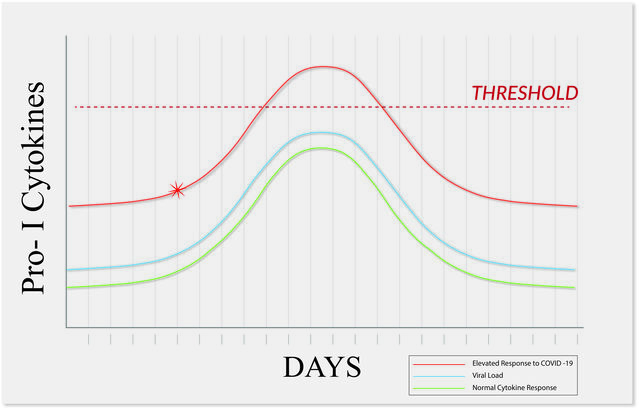
Graph designed by D. R. Clawson, MD
There are two ways to accomplish this goal. One is to arrest the activity of Pro-I’s before the level of inflammation reaches a crisis point. In the graph, the horizontal dotted line represents the level of inflammation where cytokines cause severe damage to body organs. Once that threshold is reached, mortality rate is high. The asterisk (*) represents the point where interventions to halt this “cytokine storm” are being explored. There are definite possibilities.
The other approach is to ensure that patients begin with a lower cytokine load in the first place so that, should the Pro-I’s rise as expected when faced with COVID-19, the level of elevation does not cross the critical threshold. There are strategies to this end that can be easily pursued by any of us. Presenting these approaches is the goal of this paper. First, it is important to understand the nature of threat.
Threat
Any mental or physical threat is going to be met with a defensive response from your body. Much of this is mediated through the vagus nerve, at the core of the autonomic nervous system. The response is the well-known fight, flight, or freeze reaction. Stephen Porges has presented the sequencing in his well-known Polyvagal Theory. (1)
We are familiar with the physical manifestations of an increased heart rate, sweating, rapid breathing, muscle tension, elevated blood pressure, etc. But what you may not know is that the immune system also gets fired up and mobilizes many types of cells that fend off predators such as bacteria, viruses, and cancer cells. The result is inflammation in which the “warrior cells” exit the bloodstream through widened openings in the blood vessels to destroy the invaders (antigens). Cytokines are small proteins that are the “switches," which activate and deactivate this activity.
Threat always activates pro-inflammatory (Pro-I) cytokines. Physical threats include allergens, parasites, bacteria, viruses, lions, tigers, bears, and people we perceive as dangerous. Less obvious but even more inflammatory are mental threats, because we can’t escape from them. The sustained inflammatory response destroys tissues and is the basis for chronic mental and physical disease. Examples of mental threats are memories, negative thoughts, suppressions, repressions, insecurities (social, financial, health, etc.), cognitive distortions, loss of life perspective, and purpose.

Discovery and acknowledgment of all our threats—whether real, imagined, anticipated, or repressed—is the first step toward addressing them. The second is choosing an adaptive rather than a maladaptive escape to safety, whether the threat is physical or spiritual. We are better at physical escapes to safety than we are at spiritual ones (Fredheim). If you don’t feel safe and peaceful, you are carrying elevated levels of cytokines. If you encounter the additional threat of a COVID-19 infection, you will have less chance of surviving, since you’ll already be closer to the critical threshold.
Lowering your cytokines
I am going to present an overview of the approaches. (You can access this booklet to read about each strategy in more detail.) Each has been documented in medical research to lower your pro-inflammatory response (Pro-I’s) and should improve your chances of surviving the COVID-19 infection. Using many of them will increase your odds. Conversely, ignore them at your own risk. You may have noticed in the news that the people who are dying have “risk factors.” Every one of them represents a physical or emotional threat.
Below I have outlined 10 areas to address in order to reduce your inflammatory cytokine load. I am going to summarize them, bur you can access a more detailed discussion here. Each strategy will have an effect and you should pursue as many as you can.
1. Understand and treat anxiety. Anxiety is simply your body signaling danger. It is the sensation generated by elevations of your stress hormones, activation of the sympathetic nervous system, elevated Pro-I’s, and the inflammatory reaction. It is not a “psychological issue,” although mental threats are more likely to over-stimulate the nervous system than physical ones. With the correct approach, it is solvable.
2. Get adequate sleep. At least seven hours a night of restful sleep lowers your threat response and inflammation.
3. Employ expressive writing. You can’t control your thoughts and emotions but writing them down, tearing them up and discarding the paper separates you from them. The practice has a remarkable impact on both mental and physical symptoms.
4. Practice forgiveness. Anger creates a powerful neurochemical reaction with marked elevations of Pro-I’s and inflammation. There is no shortcut to overcoming anger but it needs to be dealt with quickly. You also must address your deepest wounds. Do you want the person or situation you hate to be what ultimately kills you? Who would win?
5. Follow an anti-inflammatory diet. This can make a remarkable difference in lowering Pro-I cytokines. This is a separate goal than from losing weight.
6. Decrease stimulation of your nervous system.
- Limit watching the news.
- Avoid watching violent and over-stimulating shows, especially at night. Just witnessing violence will increase Pro-I’s (ref).
- Stop negative talk, such as complaining, gossiping, discussing your medical problems or care, giving unasked-for-advice, and criticism.
7. Maintain an exercise regimen.
- At least 30 minutes a day.
- Moderate and enjoyable.
8. Stay on top of your medical problems.
- Control your diabetes.
- Take your blood pressure and cardiac meds.
- Comply with all of your recommended medical treatments.
- Stay in touch with your doctor, even about issues you consider minor.
9. Directly address family issues. Families trigger each other, but there are effective ways to create structure that will minimize conflict.
- Living in chaos is not only unpleasant; it also has a negative impact on your health.
- Your family is usually the source of your biggest triggers.
- Be nice! Any member of your family who feels trapped is at higher risk for an illness or chronic disease.
10. Play. Having fun is one of the most powerful ways to stimulate the production of Anti-I’s and relaxation hormones.
Life is tough
It is easy to drop into living life in a survival mode. Life is tough, competitive, and challenging. For animals without consciousness, it is far more simple: You either learn the skill and cunning to survive–or not. There is also a lot of luck. Humans have the additional characteristics of language, socialization, and abstract thought. One of the curses of consciousness is that the only thing we know for sure is that we are not going to live forever. It is the ultimate fear. Yet we spend a lot of time distracting ourselves and trying not to think about it.

The paradox
Here is the paradox: The more anxious and frustrated you are, for any reason, you are adding to your threat load and there is a much higher chance that you will develop a severe disabling disease and die earlier. Additionally, while living in this state, your capacity to enjoy the time you have is compromised. You live a chaotic and reactionary life and forget to ask yourself, “Where is the endpoint?” There is none: You cannot outrace your mind.
Instead of surviving and hoping to thrive someday, it is necessary to flip the paradigm. Thriving is a learned skill similar to learning a new language. Once you have learned it, your odds of surviving improve, regardless of the circumstances–including COVID-19. Thrive and survive.
Plan A–Thrive and Survive COVID-19
Contributors: Polyvagal Work Group
David R Clawson, MD–Physical Medicine and Rehab, Seattle; Stephen Porges, Ph.D.–Distinguished University Scientist, Indiana University, Bloomington; Les Aria, Ph.D.–Lead pain psychologist, Kaiser Northern CA, Sacramento; Steve Overman, MD–Rheumatology, Seattle; Matt Lederman, MD–Internal Medicine, co-founder of Kinetin.com; Steve Lederman, MD–Cardiology; Hara Estroff Marano–Editor-at-large, Psychology Today; James Taylor, MD, Anesthesiologist, Pain physician, Pinehurst, NC.
References
1. Porges, Stephen. The Polyvagal Theory: Neurophysiological Foundations of Emotions, Attachment, Communication, Self-regulation. Norton and Co. New York, NY, 2011.




