Addiction
Can Computers Help You Quit?
Technology-assisted care in treating substance use disorders
Posted August 8, 2014
Today's blog entry is co-authored with Dr. Aimee N. C. Campbell (anccampbell@gmail.com), who is an Assistant Professor of Clinical Psychiatric Social Work in the Department of Psychiatry at Columbia University College of Physicians and Surgeons. Her research focuses on the development and testing of behavioral interventions for substance use disorders and HIV prevention and treatment, including technology-based innovations, with a specific interest in dissemination and implementation processes to increase the use and effectiveness of empirically supported treatments in community settings. Dr. Campbell completed her undergraduate training in sociology at the University of Washington and received her master’s degree and doctorate from Columbia University School of Social Work.
The article is adapted from our recent article on Rehabs.com ProTalk "Will Technology Change the Future of Addiction Treatment?"
We are getting a lot out of technology today. We use computers and smartphones to stay in touch with each other, buy things and conduct serious business. Technology is also getting smarter and smarter; recently a computer successfully masqueraded as a 13-year-old boy. Psychotherapy, on the other hand, seems like one of the most human of all activities, where personal interactions, either between patient and therapist, or between patient and patient, constitute the very core of the activity itself. The future in which technology can help us think about and address problem alcohol and drug use seems far-fetched and distant.
In fact, technology-assisted treatments are already showing great promise.
A number of psychotherapies, such as Cognitive Behavioral Therapy (CBT), motivational enhancement therapy (MET) and contingency management with money or prize-based incentives, are effective and often short-term treatments. Taking them into the community, nevertheless, has been hard for a number of reasons. There is often a lack of resources – time and money – for training, as well as for ongoing supervision to maintain adequate skill-levels. There are also limits on when and how often patients and providers can meet. Furthermore, as the Mental Health Parity and Addiction Equity Act and its extension in the Affordable Care Act are implemented, demand for substance use treatment is likely to increase.
The National Institutes of Health have recently supported a number of studies to design and test computerized systems to fill the gap that exist in clinician provided treatments. The National Institute of Drug Abuse (NIDA) and the Substance Abuse and Mental Health Services Administration (SAMHSA) are collaborating on a product to assist substance abuse treatment programs in adopting and implementing technology-assisted care.
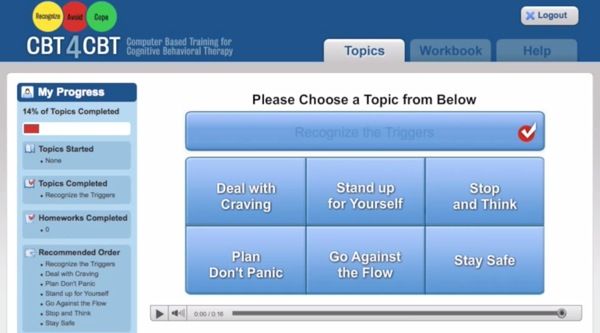
This is a screen grab from the CBT4CBT program demo video.
On the CBT treatment front, Kathleen Carroll and colleagues at Yale designed computer-based training for CBT (CBT4CBT) and applied it to a very difficult population in a NIDA-funded randomized controlled trial: patients who are cocaine dependent and also on methadone maintenance. The program is intuitive, user friendly and just makes a lot of sense: a set of computer learning games with six modules based closely on a CBT manual previously shown to be effective, with gentle introductions to the core concepts of CBT such as understanding and changing patterns of substance use, coping with craving, refusing offers of drugs and alcohol, problem-solving skills, identifying and changing thoughts about drugs and alcohol, and improving decision-making skills. (A demo is available: Figure-1.) The most impressive result: the proportion of patients who were able to achieve sustained abstinence from cocaine (i.e. 3 or weeks of abstinence): 36 percent for CBT4CBT group versus 17 percent for the treatment as usual group [1].
Our group at Columbia led a national, multi-site effectiveness trial within the NIDA Clinical Trials Network (CTN) to test an Internet-delivered behavioral intervention called Therapeutic Education System (TES). TES is a package intervention consisting of 62 interactive multimedia modules grounded in the Community Reinforcement Approach – a cognitive-behavioral intervention aimed at increasing positive reinforcement for non-drug using activities – plus prize-based motivational incentives. The modules also include relapse prevention skills and knowledge in preventing HIV, hepatitis, and other sexually transmitted infections. The TES system includes incentives for abstinence and module completion: patients earn draws from a virtual “fishbowl” and receive vouchers with either a congratulatory messages (e.g., “Good job”) or a prize (usually around $1, occasionally around $20, rarely $80–$100). Overall, TES improves abstinence in these patients, but most dramatically, TES improves abstinence among the subgroup of patients who are actively using drugs at the start of the study (i.e., had a positive urine drug screen): arguably the sicker patients. After three months of treatment, around 40 percent of the patients in TES who were positive for drugs at study entry achieved abstinence. In contrast, in the usual care group, only around 26 percent of the patients are able to achieve abstinence.

This is a screen grab from the A-CHESS smartphone application.
What about smart phones? David Gustafson and colleagues from the University of Wisconsin [3] make the observation that patients exiting residential care for alcohol use disorders are generally not offered comprehensive aftercare. This seems to run contrary to the idea of alcohol use disorder as a chronic, relapsing-remitting illness. They hypothesize that a treatment system overburdened by labor intensive programs and poor funding produces significant attrition in treatment: only 1 in 4 patients is able to maintain abstinence in the first year after treatment. To improve longer-term outcomes, they designed Addiction–Comprehensive Health Enhancement Support System (A-CHESS), a smartphone program that offers emotional and therapeutic support 24/7. A-CHESS has both a static component (eg, audio-guided relaxation) and a dynamic component: for example, the Global Positioning System can initiate an alert when the patient is close to a bar (or other designated high-risk area) and ask the patient if she wants to be there (Figure 2). In Gustafson’s latest study, patients were randomized to either receive usual care or usual care plus A-CHESS. The addition of the smartphone application improves a number of clinical outcomes, but what is most surprising is that the effect size increases in time – while at four months A-CHESS has an 8 percent improvement in achieving abstinence (not statistically significant) over usual care, at 12 months, A-CHESS has a 12 percent advantage that is both statistically and clinically significant.
These treatments have a common trait: they use technology to replicate a therapy program that is already known to work when delivered by a human and they do so with consistency and at a time and place convenient to the patient. Given the promise of these computerized interventions, we feel encouraged that technology has become mature enough to capture at least some aspect of psychotherapy that is sufficient to improve clinical outcome. Nevertheless, computer programs have their limitations. Their use still requires distribution and education, there are numerous outstanding questions about how best to integrate technology into existing treatment frameworks, and they cannot easily handle urgent and unusual situations. Skilled therapists provide a warm, connected treatment context that can never be fully replicated by devices alone. However, given the limitations on resources as well as certain advantages, such as potentially increased privacy and autonomy afforded by the computerized treatment options, we believe that these interventions can become a routine part of care delivery and implementation. Computers may not constitute the entirety of a comprehensive treatment plan for substance use disorder, but they can certainly help in getting someone to quit.
REFERENCE
[1] Carroll KM, et. al., Computer-assisted delivery of cognitive-behavioral therapy: efficacy and durability of CBT4CBT amongcocaine-dependent individuals maintained on methadone. Am J Psychiatry. 2014 Apr 1;171(4):436-44
[2] Campbell, ANC et al., Internet-Delivered Treatment for Substance Abuse: A Multisite Randomized Controlled Trial Am J Psychiatry 2014;171:683-690.
[3] Gustafson DH et al., A Smartphone Application to Support Recovery From Alcoholism, A Randomized Clinical Trial JAMA Psychiatry. 2014;71(5):566-572.




