Mindfulness
Cancer, Mindfulness, and Irritable Bowels
What I've learned over the past year of survival
Posted October 9, 2019 Reviewed by Matt Huston
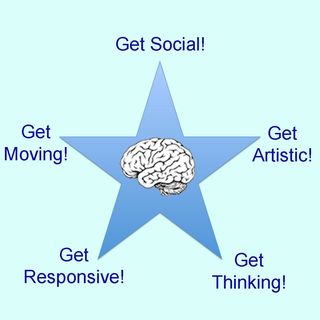
A year ago, I wrote about my time with pancreatic cancer after being given six to nine months to live, yet having survived 15 months since my diagnosis. Psychologically, I had accepted my ultimate (and presumably soon-to-occur) fate and was coping with the side effects of chemotherapy, which included significant bouts of fatigue, nausea, and lightheadedness. I was of course glad to be alive as chemotherapy had kept the cancer at bay. However, I was frustrated because I was not adhering to my own Get SMART mental health program, which is to Get Social, Get Moving, Get Artistic, Get Responsive, and Get Thinking! My cancer blog post last year was a public commitment to follow my own advice as best I could, despite my condition.
I never thought I would be writing this second post on cancer, but having survived another year, I thought I'd share a sequel to my first entry. Remarkably, I have felt well enough to lead a near “normal” life. To motivate myself to get social and get moving, I initiated plans to travel every month, even though I thought the odds were low that I would actually succeed in making these trips. Yet the planning itself was thoroughly enjoyable and, incredibly, I have been able to make all the trips to date. Destinations included “bucket list” excursions to Death Valley and Alaska. During these trips, I have visited family and friends, explored new terrain, and managed to get artistic with landscape photography. At home, I have tried to meet with friends regularly and felt enough energy to swim or tread water in my backyard pool.

I have found it somewhat difficult to initiate get responsive and get thinking programs as my primary avenues for these endeavors were teaching and writing projects that required extensive time and effort. I was asked to teach a course in the Department of Psychology at the University of Hawaii but had to decline as I could begin my downhill slide at any moment. I could write — which was my initial plan to keep mentally active after retiring from my academic position at UC Berkeley — but what a waste of time if I were to begin a book project and then get terminally ill before finishing. It was only with my wife’s encouragement that I began to write — specifically about my “personal pilgrimage,” a walk around the perimeter of my new home island, O’ahu. I did my walk in 2015 just after retiring as a way of learning about the island’s history, geography, and culture. I had always planned to write about my journey, though cancer stalled the project. My wife encouraged me to begin writing and not worry about finishing — the act of writing itself (and not the end product) would be psychologically beneficial. She was right… and amazingly I was able to finish the book this month.
It would be an Oprah moment if I could say that my Get SMART program was the sole reason for my surviving cancer this past year. However, there were other factors involved. First and foremost, the specific drugs used for chemotherapy significantly determined my disposition. After a year of one chemotherapy regimen (a combination of three drugs), I was put on a new one (two different drugs). I have tolerated this new regimen well and now realize that significant improvements in my physical and mental health coincided with this change in chemotherapy. Fortunately, this new regimen has also been effective in forestalling cancer symptoms. Over the past year, I’ve felt almost normal, whereas before it was a week of feeling ill — something akin to having the flu — before feeling well enough to do anything, and still I did not feel even close to “normal.” I believe another factor in my improved disposition was refraining almost completely from powerful anti-nausea and anti-diarrhea medications. It turns out that the side effects of these medications include fatigue and lightheadedness! It is of course a tradeoff in terms of dealing with the benefits of a drug and the problems of its side effects. In my case, I decided that feeling “with it" physically and mentally far outweighed alleviation of my intestinal issues.
As for intestinal problems, they are not trivial. For me, both chemotherapy and pancreatic cancer cause severe digestive problems, including frequent bouts of cramping, abdominal pain, bloating, diarrhea, and constipation. On occasion, I’ll take anti-nausea medication or an over-the-counter anti-diarrheal. I have, however, found a surprisingly effective mindfulness technique that helps. As many know, mindfulness training has proven to be an effective means of alleviating stress, insomnia, and other anxiety-related issues. In Buddhist traditions, meditation training includes developing an awareness of sensory experiences. One technique is to attend to your breathing, which is almost always on autopilot and thus takes some practice to keep in mind. The trick is to be mindful of the sensation, such as the pressure on your chest cavity as you breathe or the draft of air around your nostrils. I have found this mindful breathing technique to be effective around 3 a.m. when I’m suddenly awake and begin to ruminate over some stressful concern. Mindful breathing relaxes the body and prevents unwanted thoughts from entering consciousness.
Those squeamish about intestinal issues may want to skip this paragraph and just know that mindfulness helps. Recently, I have discovered that my intestinal problems — particularly constipation and diarrhea — can be significantly eased through mindfulness training. I perform my attention-to-breathing exercise on the toilet when I’m having bowel movement problems. It may seem an odd place to “meditate,” but whenever I am constipated or feel bloated, I sit on the toilet, practice my attention-to-breathing exercise and, more often than not, all systems are go! The effectiveness of this treatment was a complete surprise to me as we have been taught that visceral muscles, such as those that control the intestines, are “involuntary” and not subject to mental control. Yet I seem to be able to relax these muscles in the same way one can relax skeletal muscles. Since discovering this treatment, I have found scholarly articles on the use of mindfulness training to alleviate gastrointestinal ailments, such as irritable bowel syndrome. The evidence is there, though it is not strong, and how it works is not known.
As I stated in my first cancer blog post, I have accepted my diagnosis of terminal cancer and am realistic about my ultimate decline. I have managed to be one of the relatively few who has survived pancreatic cancer for over two years now. I feel incredibly fortunate for the time that I have had, particularly this past year when I’ve felt well enough to truly enjoy life — even more fully than I may have without cancer, as I have no qualms about exhausting my “retirement” funds for fun trips and toys (for me that's camera equipment and guitars)! Most important is that I’ve had the time with family and friends. My wife has been a saint throughout this ordeal. Moreover, I have had wonderful care from my oncologist, Dr. Ian Okazaki, and the nurses and staff at the Straub Outpatient Treatment Center (Honolulu, HI). These days I have a mantra that someone gave me recently—plan like you’ll live forever, live like you’ll die tomorrow.


