Traumatic Brain Injury
Traumatic Brain Injury (TBI) occurs when a severe jolt or blow to the head leads to brain damage. It can also result when an object, such as a bullet or shrapnel, pierces the brain.
Contents

TBIs are commonly caused by sports injuries, falls, acts of violence, and collisions involving drivers or bikers. Symptoms can appear immediately after the incident or gradually emerge in the days that follow. A concussion, which is a type of TBI, results from a hit to the head or body that causes rapid movement of the head and brain. A person should seek medical attention after a severe blow to the head, especially if it seems to have altered the person’s behavior.
Injuries are categorized as mild, moderate, or severe based on how long the person was disoriented and unconscious, as well as on brain scan results. People with TBIs can experience symptoms that differ in nature and degree. They may experience headaches, nausea, disorientation, drowsiness, trouble sleeping, slurred speech, or loss of consciousness. They may also struggle with concentration, memory, decision-making, impulse control, anger, and depression. In the sensory domain, they may hear ringing in their ears, have vision impairments, or be especially sensitive to light and sound.
TBIs are quite common. About 2.87 million emergency department visits, hospitalizations, and deaths were attributed to TBIs in the United States in 2014, according to the Centers for Disease Control and Prevention. The number of TBIs increased by 53 percent between 2006 and 2014. In 2019, there were 61,000 TBI-related deaths.
Concussions are often overlooked or misdiagnosed, but early recognition is key to recovery. According to the CDC, signs of a concussion include:
• Headaches
• Nausea or vomiting
• Exhaustion
• Dizziness
• Vision problems
• Sensitivity to light and sound
• Problems with attention, concentration, memory, and brain fog
• Atypical anxiety, irritability, or sadness
• Atypical sleep patterns or difficulty falling asleep
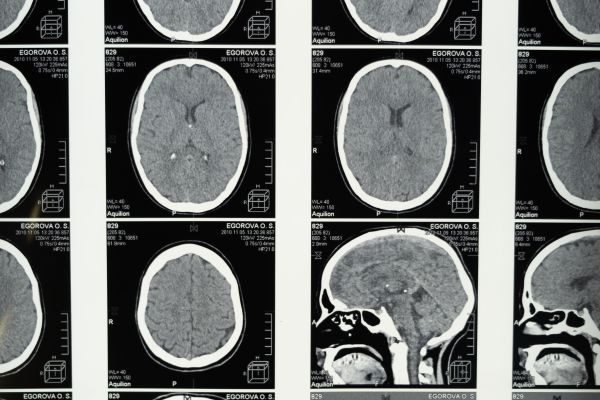
Medical professionals diagnose TBI using a variety of tests. They may rely on brain imaging through a CT scan or an MRI. They may utilize the Glasgow Coma Scale, which assesses physical abilities such as speech and movement to determine the severity of the injury (mild, moderate, or severe). They may assess behavioral measures such as speech, cognition, and memory. They may take a blood test to identify proteins that are often elevated after a head injury. Diagnosis can be difficult because it can sometimes be challenging to distinguish between TBI and other conditions such as post-traumatic stress.
Post-concussion syndrome refers to symptoms of a concussion that persist after the typical recovery window, often three to six months. The symptoms are those that follow a concussion, such as headaches, dizziness, sensory sensitivity, and trouble concentrating. Many people do not realize they had a concussion or were misdiagnosed, so they may not have sought treatment for the injury.
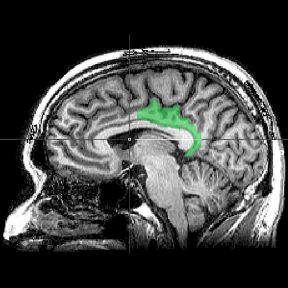
A sudden jolt, such as those that occur in concussions, can send the delicate brain crashing into the hard skull that surrounds it. This can cause the brain tissue to bruise or swell where it collided with bone. It can also strain a part of neurons called axons, which facilitate communication between brain cells. The force can stretch and rip axons apart, leading them to release chemical toxins that kill other brain cells.
People often think of sports injuries and car accidents when considering a brain injury, but many other incidents can lead to TBI as well. Domestic abuse, falling on the stairs or around the house, falling outside such as slipping on ice, and injuries sustained during natural disasters can also lead to concussions.
Non-traumatic brain injuries, also called acquired brain injuries, encompass all forms of brain damage that result from factors other than external blunt force. This category includes stroke, aneurysm, oxygen deprivation, including hypoxia and anoxia, toxin exposure such as lead, brain tumors, viruses, and encephalitis. Non-traumatic brain injuries can spread from one brain region to another, while traumatic brain injuries cannot. Traumatic and acquired brain injuries produce similar symptoms; treatment may be similar but target different underlying problems.

Head injuries have the capacity to alter behavior, and those changes depend on the severity and number of injuries. Short-term changes include feeling dizzy, confused, and exhausted. An injured person could have a headache, nausea, blurred vision, ringing in the ears, and sensitivity to light and sound.
Most people recover smoothly within a few weeks and show no permanent harm. But in some cases, lasting changes occur. People who suffer a TBI may lose the ability to concentrate as intently as they did previously, which may manifest at work, in conversations, or in household tasks. They may struggle to remember events or facts. Personality may shift as well: One may become more irritable, angry, or impulsive, or less able to exercise self-control. TBI sufferers may struggle with depression and anxiety, as well as sleep disturbances.
Repeated concussions can lead to Chronic Traumatic Encephalopathy (CTE), a neurodegenerative disorder that may be linked to severe changes in memory and impulse control, anxiety and depression, and suicidal thoughts or behavior. Many prominent athletes have posthumously been diagnosed with CTE—which has triggered a global discussion about the science, ethics, and commercialization of football and other contact sports.
Yes, there seems to be a clear connection between TBI and psychiatric symptoms. A 2013 study that followed 1.4 million Danish citizens found that individuals with TBI were four times more likely to develop a mental illness. People who received a TBI were 65 percent more likely to develop schizophrenia, 59 percent more likely to develop depression, and 28 percent more likely to develop bipolar disorder.
Another study found that experiencing depressive symptoms after a head injury is more common than not; the prevalence of depression after TBI was greater than 50 percent. Yet another found that people who received a concussion in the past were three times more likely to die by suicide.
Head injuries can cause subtle or pronounced changes in personality. In more severe cases, the injured person may have angry outbursts or make impulsive decisions. The person may be frustrated when reminded of their losses, for instance, the inability to drive. As one woman described after her husband’s brain injury, “It was as if two versions of Alan resided within him. One was rational and easy-going, but the other was frightening and even dangerous at times.”
These changes can lead to distrust due to unpredictability, emotional pain for the caregiver, unresolved conflicts, and considerations of physical safety. Anger management strategies can help address these challenges and repair relationships after a TBI.
Chronic Traumatic Encephalopathy (CTE) and concussions are separate entities. CTE is a chronic neurodegenerative disorder, which goes through a number of phases that can lead to a myriad of symptoms and behavioral problems. CTE occurs in those with repetitive brain trauma, but genetic and other factors may contribute to the diagnosis as well. Not every individual who has a sports-related concussion will develop CTE.

It's important to seek medical attention for any head injury, even if there are no immediately apparent symptoms. (Brain swelling may take hours or longer to manifest.)
Mild TBIs, which include concussions, are treated with rest and over-the-counter medication for headaches. The person can then gradually resume physical and mental tasks in accordance with a doctor's guidance, so as not to overwork the brain or prevent a full recovery.
Moderate and severe injuries are treated with a combination of medication, surgery, and rehabilitative therapies. Patients are first stabilized to prevent further injury, which may include controlling blood pressure and ensuring proper blood flow to the brain. Surgery may be necessary to repair a fracture in the skull, remove blood clots, or drain excess fluid from the brain. Medications may be prescribed to prevent blood clots (anticoagulants), stop seizures (anticonvulsants), or address anxiety and depression (antianxiety and antidepressant medications).
Patients may engage in a variety of therapies. Physical therapy can help one regain strength and movement, occupational therapy can restore the ability to carry out daily tasks, speech therapy can improve communication, and cognitive therapy can hone memory and concentration.
Medical professionals can adhere to guidance that can increase the chances of a successful recovery. This includes:
1. Neuroprotection through restorative interventions: stabilizing the brain immediately after the injury through measures such as rest at home or managing blood pressure, sedation, and ventilation at the hospital.
2. Understanding the natural history of the recovery process for each individual: tracking and personalizing the recovery process rather than treating patients indiscriminately.
3. Implementing the appropriate therapeutic modality throughout injury and recovery: introducing interventions such as medication and rehabilitative therapies.
4. Determining what compensatory mechanisms the nervous system develops during healing and providing appropriate intervention: for example, dizziness may signal that the body isn’t ready for certain stimuli or depression may signal that the patient is realizing the extent of their limitations.
5. Implement an appropriate rehabilitation process: rehabilitation may include working to restore previous functions, compensating when function can’t be restored, or adapting the person’s environment.
People may not seek treatment for a head injury because the symptoms can be hard to identify and objectively measure. Awareness of the importance of treating a head injury is often relatively low. In the case of college or professional athletes, their financial future may be on the line, they may not want to let down their teammates, and they may be worried about appearing “weak” to others or themselves. Countering these narratives is critical so that athletes and others with TBI can recover properly.
While the physical trauma of a brain injury takes center stage after an injury, emotional trauma is often dismissed or neglected. Patients can have a range of symptoms that are difficult to navigate or threaten their sense of independence and identity, ranging from confusion and dizziness to the inability to walk or control bowel movements. The term “walking wounded” refers to individuals with injuries that leave minimal to no scars but have significant post-trauma difficulties (similar to the label invisible illness).
An invisible disability or illness is a medical or psychological condition that isn’t obvious to others. Aside from daily physical challenges, one of the most difficult consequences is the lack of understanding from others. Those with invisible disabilities are frequently faced with comments, judgments, and rude questions, which can lead to relationship problems as well as anxiety, guilt, and exhaustion.
Strategies to cope with an invisible illness or injury include letting go of expectations, seeking support from friends and family, practicing self-compassion, identifying activities that bring joy, picking your battles, spreading awareness, and adhering to a plan to manage symptoms.
Immediately following a brain injury, loved ones should help the person seek diagnosis and treatment, both logistically and emotionally. In the recovery phase, loved ones should educate themselves about TBI, assist with daily functions, support their loved one emotionally, and practice patience and self-care throughout the process. Family and friends may struggle with how the person changes, perhaps becoming irritable and moody with poor frustration tolerance. Patients and their family members can learn to integrate both the good and the bad, and discuss these challenging dynamics openly as they evolve.