Psychiatry
Psychiatry is a specialty of medicine that focuses on researching, understanding, diagnosing, and treating diseases of the brain and disorders of the mind and behavior. Psychiatrists diagnose and treat a wide range of conditions, from Alzheimer’s disease, anxiety, and autism to mood disorders, Munchausen syndrome, psychosis, and suicidality. As physicians, psychiatrists are trained to recognize the many ways general physiologic processes and pathologies can influence mental functioning—and vice versa.
Practitioners are physicians who typically work in or are affiliated with medical settings. Psychiatry also has a number of fields of subspecialization; addiction psychiatry, child and adolescent psychiatry, forensic psychiatry, geriatric psychiatry, and neuropsychiatry are the best known.
Some psychiatrists devote themselves exclusively to research. Others may be affiliated with medical institutions where they both conduct research and evaluate and treat patients. Others may engage exclusively in patient treatment, in outpatient settings such as independent clinical practice, in a group practice affiliated with other physicians, or in a psychiatric facility. Many clinical psychiatrists have attending privileges in hospitals to accommodate patients needing care and supervision or experiencing a psychiatric emergency.
All psychiatrists begin care with an extensive evaluation of each patient that can provide important clues to the source and nature of the disorder. Psychiatric evaluation includes an interview in which the patient is asked to describe symptoms, personal and family history, medical history, and may include blood and other tests. Psychiatrists pay attention not only to what is said but to the emotional tone of responses, the cognitive factors informing them, and the behavior accompanying them.
Psychiatrists have at their disposal an array of treatments ranging from psychotherapy to pharmacotherapy to somatic therapies, including brain stimulation. Increasingly, for example, psychiatrists report paying attention to the reciprocal influence of bodily states on brain function and to gut health as a significant contributor to mental health, both of which are flourishing areas of research. Advances in the understanding of the role of diet, sleep, and regular physical activity on well-being in general and mental functioning, in particular, are also finding their way into patient management as well.
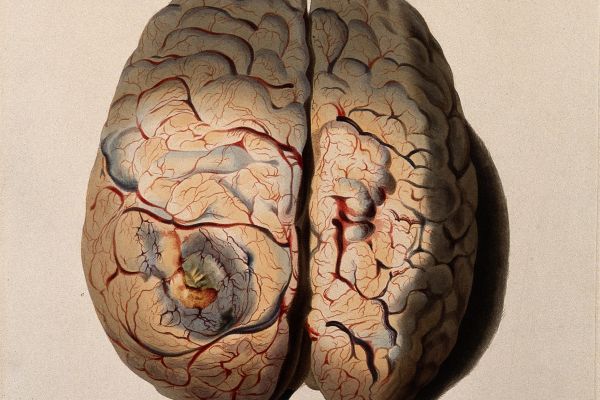
Tools such as neuroimaging may sometimes be helpful in diagnosis but currently are more widely used in clinical research to further the general understanding of mental disorders and the neurobiological dysfunction that gives rise to or accompanies them.
Contents

Most psychiatrists have subscribed to the biopsychosocial model of illness, which posits that biology, psychology (including thoughts and emotions), and social factors (relationships, socioeconomic conditions, culture) interact to influence health, disease, and human development.
One of its principal corollaries is that mental disorders have multiple causes: From anxiety to schizophrenia, symptoms of mental illness and distress arise from an array of factors, including stress reactivity, memory and other mental processes, social relationships, lifestyle including nutrition, and general environmental factors, including racism. The interplay and relative contribution of each factor vary from individual to individual.
Because of the enormous complexity of the human mind and the influences on it, disorders can often express themselves in a multitude of ways, and indeed, symptoms can shift over time.
Because of its power to relieve anxiety and induce states of calm, the physician-patient relationship—sometimes referred to as the therapeutic alliance—can be utilized to play a significant role in the healing process. It sets the stage for patient healing regardless of the disorder.
Classification of mental disorders, codified in the Diagnostic and Statistical Manual of Mental Disorders, now in edition 5 (DSM-5), is an ongoing and often “messy” process based on evolving understanding of the brain and mind; the classification of disorders contributes to correct diagnosis of problems and appropriate treatment.
The unconscious mind is not a source of dark desires waiting to betray you despite your best intentions. It is a complex system of activity in which perception, evaluation, motivation, and other processes are constantly working outside of conscious awareness to influence physical and emotional state and guide behavior. Nevertheless, with deliberate effort, those processes can sometimes be made accessible, and one of the roles of psychotherapy is to help people do so.
Many mental disorders, including anxiety and depression, are characterized by dysfunction of the neural circuitry interconnecting areas of the brain that mediate stress responsiveness (the amygdala), memory (the hippocampus), and emotion regulation (the prefrontal cortex). Identifying the neural circuity underlying complex brain functions such as mood regulation is providing new ways of intervening in disorders, including the development of ever more precise methods of brain stimulation as a treatment for depression and other conditions.
There can be much overlap in symptoms among psychiatric disorders. For example, psychosis may be the hallmark of schizophrenia, but similar delusions, hallucinations, and disorganized thinking are present in up to 20 percent of patients with major depressive disorder. In addition, such symptoms are common among those with bipolar disorder. When is distractibility in children a sign of ADHD, or when is it a sign of mania in childhood bipolar disorder?
Chronic stress is increasingly recognized as a source of many psychiatric symptoms and disorders. It is experienced by the body with extensive changes in physiology, including the production of pro-inflammatory cells and signaling compounds that alter the functioning of nerve circuits in the brain. One effect is to turn on unrelenting cascades of negative thoughts, feelings, and expectations, symptoms that give rise to anxiety, depression, suicide, and other distressing conditions.
Mental suffering is different from other forms of illness. When your body is sick, it impacts your body. When your mind is sick, it impacts your entire person—the very essence of who you are, of what makes you you. Mental pain brings with it a flood of negative feelings that reach deep into one’s sense of self—anguish, fear, loneliness, helplessness. Because the neural pathways that underlie emotional pain are shared with those that express physical pain, the distress is felt physically as well, often in some indefinable way beyond the reach of language. It is both physiological and psychological. And because pain is so inescapably subjective, it is deeply isolating. As profoundly unsettling as mental pain is to those experiencing it, it can make them reluctant to trust the very people who can help them—mental health care providers.
Using information from a person’s general medical history and current interview, a psychiatrist will inquire about both family history and personal history. Patients are asked about physical and mental health symptoms and medications (if any), troubling thoughts and behaviors, situations that bring on the symptoms or make them worse, how often symptoms occur, how long they last, how they affect work or school performance, relationships with others, and involvements with others and activities.
They will be asked about their upbringing, their current life and relationships, sources of stress, and troubling experiences. They may be asked to describe the degree of pain they feel or to represent it on some visual scale. The psychiatrist is paying attention not only to the answers to questions but making observations about a patient’s level of consciousness, appearance, motor activity, emotional state, expressions, mood and affect.
The mental status examination takes place during the course of a clinical encounter and includes general observation of patient behavior—the rate of speech, appropriateness of conversation—as well as specific focus on any of various components of cognitive function—attention, memory, executive function, thought processes, and more. Patients may be asked to recall specific events, to repeat a sequence of words, to solve problems, or to describe any thoughts they have about others’ intentions toward them. It is used to help distinguish between general systemic conditions as well as neurologic and psychiatric disorders.
The criteria for diagnosis of mental health disorders are laid out in The Diagnostic and Statistical Manual of Mental Disorders, or DSM. Reviewed and modified periodically by experts, in response to new information and understanding of mental dysfunction, the DSM is now in its fifth edition. DSM-5 details more than 20 broad categories of mental disorder:
- Neurodevelopmental disorders, including intellectual disabilities, autism spectrum disorder, ADHD, tic disorders such as Tourette’s syndrome
- Schizophrenia and other psychotic disorders
- Bipolar disorders
- Depressive disorders
- Anxiety disorders
- Obsessive-compulsive and related disorders, including hoarding and trichotillomania, or hair-pulling
- Trauma- and stressor-related disorders, including PTSD and attachment disorders
- Dissociative disorders
- Somatic symptoms and related disorders, including illness anxiety disorder (hypochondria)
- Feeding and eating disorders
- Elimination disorders, including enuresis (bedwetting)
- Sleep-wake disorders, including insomnia and narcolepsy
- Sexual dysfunctions, including desire, arousal, and erectile disorders
- Gender dysphoria conditions
- Disruptive, impulse control, and conduct disorders
- Substance-related and addictive disorders
- Neurocognitive disorders including Alzheimer’s disease
- Personality disorders
- Paraphilic disorders, including voyeurism, exhibitionism, and fetishistic disorder
- Medication-induced disorders, including tardive dyskinesia
- Relational problems, abuse and neglect, and partner violence
For each disorder in each category, the DSM specifies the symptoms that characterize the disorder and the frequency with which they must be present to be considered a disorder. After all, everyone gets depressed sometimes, but not everyone experiences relentless mood disturbance that disrupts a person’s life. In almost all categories of disorder, diagnosis can be made only if symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
Although the DSM catalogs behavioral symptoms, many of which overlap disorders, the future of psychiatry may rely more on objective criteria for diagnostic precision, specifically on the biologically based signs of a disorder. For example, neuroimaging procedures and other techniques allow doctors to look directly at the brain, and refinements in imaging technology promise to allow accurate detection and diagnosis of mental illness—to determine, for example, which brain cells might be misbehaving and under which conditions. Much research in psychiatry is devoted to the search for biological markers that are indicators of specific pathology and can help clinicians distinguish between disorders and apply the most targeted treatment.
The cornerstone of all healing is the physician-patient relationship; this is considered to be the case in all of medicine, but it especially applies in psychiatric disorders. Research demonstrates that a strong, trusting bond between doctor and patient has measurable biologic effects, inducing a state of physiologic calm; the system is shifted away from the production of stress-related substances that set the body up for defense, invariably at the cost of damage to the brain as well as body tissue. The doctor-patient relationship is the primary conduit of psychotherapy, but it also sets the stage for recovery when biology-based treatments are used.
For many psychiatric conditions, the standard of care is combination therapy—psychotherapy in tandem with medication. The most commonly prescribed classes of psychotropic drugs include:
Antidepressants. Developed to treat depression, antidepressants are also commonly used in the treatment of anxiety disorders, including panic. The most widely prescribed antidepressants are known as selective serotonin uptake inhibitors (SSRIs), and they were originally thought to work by boosting levels of the neurotransmitter serotonin in the brain, but it has never been clear how the change in neurotransmitter levels creates symptom relief. The prototype drug of this group is Prozac.
Anti-anxiety medications, or anxiolytics. Used to treat anxiety disorders, such as generalized anxiety disorder and panic disorder, anxiolytics aim to calm the nervous system. Tranquilizers such as Xanax and Klonopin are popular drugs in this group. In fact, Xanax is the most widely prescribed psychotropic medication of all, outpacing any of the SSRIs. Nevertheless, the SSRI antidepressants are among the drugs most commonly prescribed long-term for anxiety, a condition that shares many features with depression. Typically, SSRIs are prescribed in higher doses for anxiety than for depression.
Mood-stabilizing medications. Mood stabilizers—lithium is the classic agent—are commonly prescribed to prevent mood swings in bipolar disorder. They are also sometimes used along with antidepressants to treat depression.
Antipsychotic medications. Antipsychotic drugs clarify thinking and are typically used to treat psychotic disorders such as schizophrenia. They are also increasingly used to treat bipolar disorders or used with antidepressants to treat depression.
Stimulants. Stimulants are typically prescribed—paradoxically—for the treatment of ADHD (along with psychotherapy and lifestyle changes). The most widely used drugs are the nervous system stimulant amphetamine Adderal and Ritalin, a synthetic nervous system stimulant. The stimulants act by increasing brain levels of the neurotransmitter dopamine, which boosts motivation and attention.
Sometimes called talk therapy, or just therapy, psychotherapy consists of a series of structured meetings with a professional trained to understand the operation of the mind and improve human functioning, In general, therapy works on several dimensions of experience at one time—to relieve a patient’s feelings of distress, to resolve problems, to provide insight into one’s nature, and to bolster coping strategies.
Conducted largely through expertly guided discussion, therapy is a powerful enough tool to change the brain. Studies show it produces lasting changes in the architecture and functioning of the brain, notably in those areas that control thoughts and memories. Therapy can alter nerve circuitry and strengthen connections between regions of the brain, dampening signals of negativity that make so many conditions feel so oppressive and restoring a sense of control.
While psychiatrists are generally trained to conduct therapy themselves, more commonly today they work in tandem with psychologists and other mental health clinicians to administer this treatment. Patient and therapist work collaboratively and periodically assess improvement.
It is important for patients to work with a therapist who has expertise with their type of problem. One way of finding a therapist is by using an online Directory). Or the patient’s insurance company may have a list of covered providers.
There are many types of psychotherapy, each putting the emphasis on differing aspects of or strategies used in the treatment. They have been rigorously tested on large numbers of patients over the years and found effective. These are among the most common types of therapy.
Cognitive and Behavioral Therapy (CBT). Likely the most widely used and validated form of psychotherapy today, CBT is a relatively structured course of treatment (5 to 20 sessions) that is present-focused and aimed at dismantling the near-automatic thinking patterns that commonly give rise to emotional distress. Applied in depression, anxiety, eating disorders, and many other conditions, it teaches patients ways of noticing and curbing distressing thought patterns and offers skills for regaining control in stressful experiences. Patients are often given “homework” assignments for practicing in their everyday lives the skills they learn in session.
Acceptance and Commitment Therapy (ACT). Acceptance and commitment therapy is a form of CBT that draws strongly on mindfulness and other techniques to diffuse negative thinking, accept life’s challenges, relieve suffering, and gain skills for handling difficulties.
Dialectical Behavior Therapy (DBT). A cognitive-behavioral treatment for complex mental disorders, DBT was initially developed to treat chronically suicidal patients. It has since been adapted to treating patients with borderline personality disorder and others with “seemingly intractable behavioral disorders involving emotional dysregulation,” according to its developer. It has components of individual therapy and group therapy.
Interpersonal Therapy (IPT). Initially developed to treat depression, IPT is a structured, brief (12 to 16 weeks) therapy aimed at resolving the relationship problems that are typically the catalyst for depressive episodes.
Family Therapy. Based on the knowledge that families powerfully—and often silently—shape individual as well as relationship behavior, family therapy, or family systems therapy, is conducted with all or most members of a family attending each session, with the goal to resolve conflicts and improve patterns of functioning for everyone.
Psychodynamic Therapy. Psychodynamic therapy is a modern evolution of psychoanalysis, emphasizing self-examination to get at the roots of emotional suffering. Unlike traditional psychoanalysis, the therapist is usually an active guide in the discussions. It is more likely than other therapies to explore past experience as a means of gaining insight into current behavior patterns.
Sometimes the only way to relieve suffering is to directly alter the transmission of nerve impulses in areas or circuits of the brain that control specific functions. With refinements in technology that allow for precision targeting of nerve nodes, such treatments, using the permanent placement of tiny electrodes or the repeated use of magnets, are becoming increasingly common for a number of disorders, particularly those that are not relieved by other methods of treatment.
Electroconvulsive therapy has long been the treatment of last resort for those experiencing intractable depression. With the patient under general anesthesia, an electrical current is applied to the brain with the intent of inducing seizures that “reset” neural transmission in the brain. Treatment is often administered in a series over the course of a few weeks. Memory loss is a common after-effect of the procedure. The treatment is not a cure, and patients may undergo additional courses of ECT over time. It is estimated that each year, 100,000 patients, either with major depression or severe bipolar disorder, undergo such treatment in the U.S.
Transcranial magnetic stimulation (TMS) is a noninvasive recurring treatment for depression and anxiety in which a magnet is precision-placed over a specific area of the head to activate nerve cells in areas of the brain known to be involved in those disorders. Patients are fully awake and alert during the treatment.
Deep brain stimulation involves the surgical implantation of tiny electrodes to a very specific cluster of neurons in order to stabilize the generation of electrical impulses by which nerve signals are transmitted. It is sometimes used as a treatment for obsessive-compulsive disorder, Tourette’s syndrome, and intractable depression.
Vagus nerve stimulation (VNS). Stimulation of the vagus nerve is a means of regulating the excitability of nerve cells without inducing seizures. The vagus nerve, which begins in the brainstem, has many branches, and vagal nerve stimulation is used medically to normalize heart rate in people with cardiac arrhythmias. It is also used in regions of the brain to control refractory epileptic seizures. Because depression is associated with the overactivity of certain brain circuits, VNS is also sometimes used to relieve unrelenting depression. A small mechanical device delivering intermittent electrical impulses to the vagus nerve is implanted inside the chest cavity or noninvasively affixed to the skin.
There are other nonmechanical ways of stimulating the vagus nerve—such as deep breathing techniques—and they are increasingly used to subdue states of anxiety and unease. Most versions of cognitive behavioral therapy teach such calming techniques as an important stress-reduction skill.
- The role that the brain plays in interpreting information about and regulating the internal state of the body is increasingly under scrutiny as a significant factor in psychiatric illness. Studies show that disturbances in so-called interoception occur in schizophrenia, bipolar disorder, anorexia, anxiety, and major depression, and involve a specific area of the brain.
- The role of medication in psychiatric conditions has long been a contentious matter, especially for children. Although many and perhaps most psychiatrists believe that medication should generally be accompanied by psychotherapy, the structural economics of practice and reimbursement have so weighted that matter that the 15-minute appointment for a “med check” is regarded as standard care. Although psychiatrists are often in a private tug of war between psychological thinking and treatments and psychopharmacologic thinking, training is now weighted towards the latter.
- One of the longstanding criticisms of psychiatry is that it blunts forces for social change by dealing with individuals whose mental distress results, in whole or in part, from social ills such as poverty and discrimination, and attempts to undo the damage of such ills on an individual-by-individual basis rather than by changing the conditions that give rise to distress. Psychiatrists themselves debate how much of a role they should play in alleviating social ills, and just as the broader culture varies over time in the emphasis it gives to any of the varied influences on mental health, so does the field of psychiatry. Nevertheless, the subspecialty of Community and Social Psychiatry specifically addresses mental health issues of at-risk populations, and some departments of psychiatry put special emphasis on it. It is likely that debate will never end about the reach of responsibilities of those whose job is to relieve mental suffering.
- Some psychiatric conditions tend to run in families, and psychiatric patients have a disproportionately large number of first-degree relatives with mental health disorders. A search for the shared genetic vulnerability has proved overly simplistic and has given way to a more complex search for factors other than genes that influence the transmission of disorders in families.
- The roles of such general physiologic processes as inflammation and cellular metabolism in psychiatric disorders are relatively new targets of research. Both processes, for example, are implicated in mood disorders and Alzheimer’s disease.
- The role of the gut—and especially the composition of the gut microbiome, which is heavily influenced by diet—in mental health and disease is under study as evidence shows that there are many direct and indirect pathways of communication between the gut and the brain. Scientists are exploring the role of diet in autism, bipolar disorder, and other conditions.
- The application of physical approaches such as stimulation of deep brain tissue through transcranial magnetic stimulation (TMS) has been in clinical use for the treatment of resistant depression since 2008. Its effectiveness for other conditions such as obsessive-compulsive disorder (OCD) is now under study.
- Research into the clinical application of psychedelic drugs is accelerating so quickly it is being called a paradigm shift in psychiatry. Early results show that short-term use of psychedelic agents in combination with intensive psychotherapy, under study for the treatment of refractory conditions such as PTSD, anorexia nervosa, OCD, and substance abuse disorders, as well as depression, can create rapid and dramatic shifts in neural, cognitive, and behavioral flexibility.
- The exact nature of autism and what underlies its array of symptoms is still unclear. Nonetheless, some progress exists in identifying distinctive biological markers of the disorder, identifying those at risk, and developing effective treatments.
Both clinical psychiatrists and clinical psychologists have as their goal the alleviation of mental distress and suffering. And both psychologists and psychiatrists are major participants in research about mental illness and health and in developing new treatments. Both must be licensed in the state where they practice.
But in practice, the tools they have at their disposal differ. While both can conduct psychotherapy, psychiatrists are physicians who can prescribe medication. With a health care system set up to favor the dispensing and management of medication for the treatment of disorders—often to the frustration of those practicing medicine in the system—rather than to the dispensing of appropriate care established and delivered through a trusting physician-patient relationship, that becomes a significant clinical difference. Only a small percentage of psychiatrists today conduct psychotherapy. In most mental health settings, therapy is typically administered by a psychologist or other psychotherapist, often in consultation with a psychiatrist administering medication.
Other differences reflect the origins of the two disciplines. Psychology has its origins in philosophy, and psychologists study the development of the mind and the nature of consciousness, the development of emotions and cognition, the development and nature of personality. Traditional psychology training programs offer a Doctor of Philosophy (Ph.D.) degree and have an orientation to research and training in scientific methodology; a research-based dissertation is a requirement for the degree. Knowledge of psychology is useful to many human endeavors, from education, including animal training, to the design of products to the management of organizations. Psychologists work in many fields besides those related to health care.