Genetics
Erectile Dysfunction: What Causes It and What Could Fix It
Exploring the biological background of failed erections.
Posted November 10, 2020 Reviewed by Ekua Hagan
Failure to achieve erection afflicts men around the globe. Formerly called male impotence and now officially known as erectile dysfunction (ED), it is disturbingly common. A 2019 global review by Anna Kessler and colleagues reported rates ranging from 13% to 71% for individual countries. Prevalence for North America was 21% and for diverse European countries between 17% and 65%.
ED clearly has multiple causes, with both biological and psychological factors contributing. It is, for instance, more common in men with depression. Although broad-based treatment has the best prospects of success, well-defined biological factors are involved.
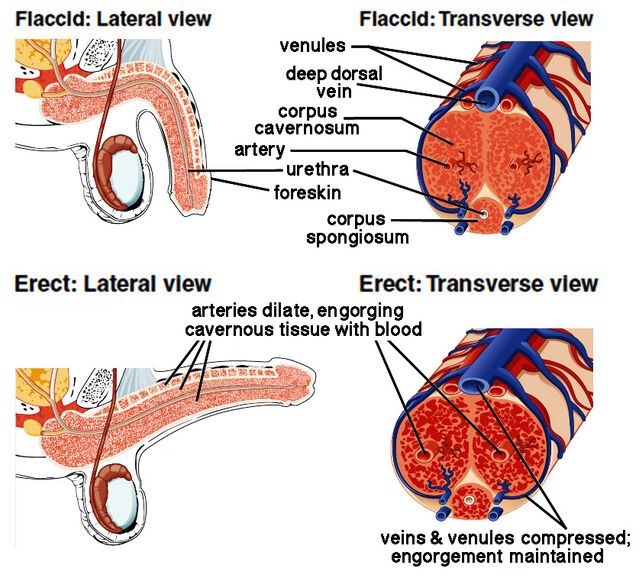
Anatomy of erection
Three inflatable compartments extend along the human penis. A bulky cavernous body (corpus cavernosum) is present on either side, while a smaller spongy body (corpus sponglosum) lies beneath, surrounding the duct carrying urine from the bladder (urethra). A build-up of arterial blood (vasocongestion) engorging all three compartments causes erection. The blood-filled chambers compress the thin-walled veins, maintaining erection by preventing blood from leaving the penis.
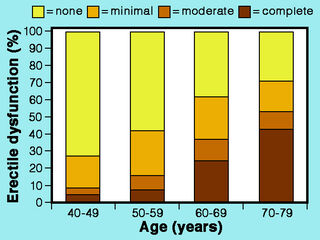
Erectile dysfunction
Some degree of ED affects many men. The 2019 review by Anna Kessler and colleagues noted that all studies reported increases with age. In fact, the continuous aging of the global population has been linked to a worldwide rise in ED. In 1999, Işik Ayta and colleagues estimated a global prevalence of 152 million and predicted that this will double by 2025. In addition to general aging, ED has been linked to cardiovascular disease, diabetes, prostate complaints, psychiatric disorders, alcohol, smoking, use of certain drugs (e.g. antidepressants), lack of physical exercise, and low testosterone levels. But the primary factor is hardened arteries (atherosclerosis), impairing peripheral blood flow and potentially leading to heart attacks or strokes.
ED is connected to atherosclerosis because it reflects changes in blood flow to and from the penis. It is hence likely to be linked to circulating cholesterol levels as well. Ming Wei and colleagues reported the results of a study designed to test this in a 1994 paper. They analysed data from 3,250 men aged 26-83 years who did not have ED when first examined and were subsequently monitored for an average of 2 years. During follow-up, ED was diagnosed in 71 of those men. After allowing for various confounding factors, the overall risk of ED was found to increase significantly with total cholesterol. By contrast, the risk decreased significantly as high-density lipoprotein cholesterol increased.
Animal models
Animal models often contribute significantly to the development of medical treatments. Although animal examples of ED are understandably difficult to find, exceptions exist. In 2012, James Williams and colleagues reviewed information from rodents, rabbits, dogs, and non-human primates. As Kurt Weingand recounted in a 1989 paper, long-tailed macaques are a prime case. This condition was deliberately induced in captivity by feeding macaques a cholesterol-rich diet for 2-5 years. Especially because blood vessel lesions resemble those in humans, these macaques became a widely used primate model for hardened arteries.
After observing long-tailed macaques with diet-induced atherosclerosis, in 1984 Michael Adams and colleagues reported on failed erection and ejaculation in adult males in which hardened arteries impeded blood supply to the penis. Compared to control males, macaques with atherosclerosis showed marked deficits during sexual interactions with receptive females. Examination of blood vessels supplying the penis revealed blockages hindering the marked surge in blood-flow needed for erection.
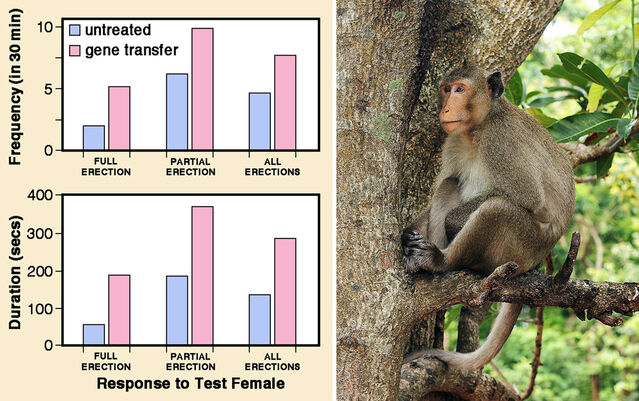
Some 25 years later, this primate model yielded dividends in a successful gene transfer experiment. George Christ and colleagues observed eight male long-tailed macaques with diet-induced atherosclerosis, recording baseline data for their sexual behaviour when individually caged with a test female. A vector carrying a gene specific for enhancing smooth muscle function was then injected into the cavernous bodies of the penis of each male. Following gene transfer, “dramatic changes” occurred in male sexual behavior and erectile function: Frequency and duration of erections increased significantly.
In the interim, one might have hoped to see this promising approach routinely applied to treat human ED. However, gene transfers have rarely been evaluated in clinical trials as yet and crucial safety concerns remain to be addressed.
A pharmacological breakthrough
Meanwhile — confirming the maxim that many important discoveries are accidental — a chance finding led to a major advance in ED treatment. In the 1990s, clinical trials of the drug SILDENAFIL were initiated to assess its capacity to reduce high blood pressure and alleviate inadequate blood flow through the heart. It turned out that the drug brought no benefit for either condition, but researchers noticed that many men had erections (sometimes long-lasting) during tests. A clinical trial launched to assess the capacity of SILDENAFIL to boost erections in men with ED yielded the first really effective oral treatment. Approved by the US Food and Drug Administration in 1998, it was marketed as “Viagra." Annual sales of Viagra and related drugs in the USA now exceed a billion dollars, with reported effectiveness of 80% in treating ED.
SILDENAFIL and allied agents — VARDENAFIL (e.g. Levitra) and TADALAFIL (e.g. Cialis) — belong to a class known as phosphodiesterase type 5 inhibitors. They act on smooth muscle cells lining blood vessels in the body, among other things dilating the cavernous bodies in the penis and facilitating erection. A 2012 review by Giuseppe Lombardi and colleagues reported positive benefits from treating ED in patients with spinal cord injury, Parkinson's disease, and multiple sclerosis.
Erectile dysfunction and vitamin D
My previous two blog posts discussed the wide-ranging impacts of vitamin D deficiency on human health ("Vitamin D Is Essential for Human Reproduction" and "Skin Colour, Vitamin D Deficits, and Disease Risks"). A lengthy list of effects of low circulating vitamin D levels includes hardened arteries, hypertension, and heart attacks. So links to ED are only to be expected.
In a 2014 paper, Alessandra Barassi and colleagues examined blood levels of vitamin D in 143 ED patients. They used echo‐color‐Doppler scans to examine the penis before and after injecting prostaglandin E1, a hormone known to trigger erection. Almost half the patients had very low blood levels of 25-hydroxyvitamin D3 under 20 ng/mL, while only a fifth had levels above 30 ng/mL. Moreover, patients with severe ED had significantly lower levels than those with mild ED. Scans revealed that ED attributable to arterial defects was significantly almost twice as common among patients with blood levels below 20 ng/mL.
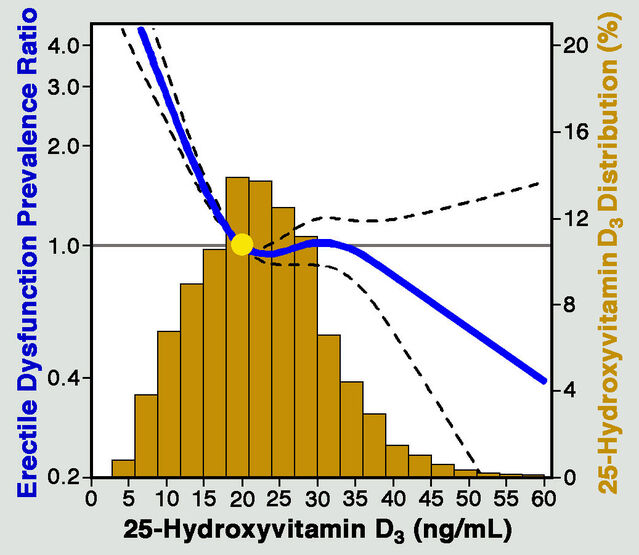
In 2016, Youssef Farag and colleagues published additional information on the association between ED and vitamin D deficiency, having conducted detailed statistical analyses of data for almost 3400 men in the US National Health and Nutrition Examination Survey (2001-2004). Analysis allowing for potential confounding factors showed that men with vitamin D deficiency (below <20 ng/mL) had a significantly higher prevalence of ED than men with blood levels of 30 ng/mL or more.
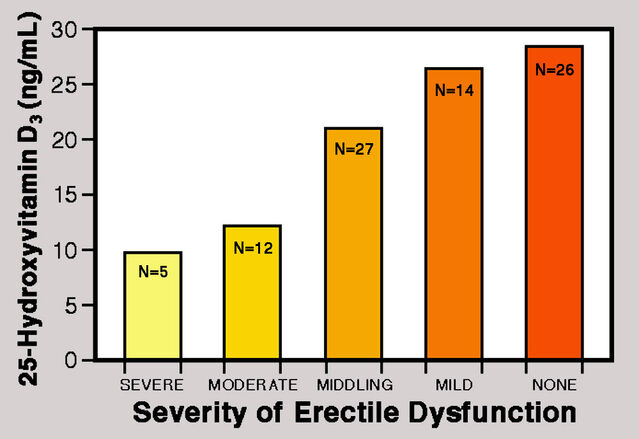
A 2020 paper by Ion Dumbraveanu and colleagues confirmed that finding after comparing 58 ED patients with a control group of 26 healthy men. They found a significant inverse correlation between the severity of ED and vitamin D levels. Moreover, vitamin D and testosterone levels showed a significant positive association.
These findings all involve correlations, which cannot distinguish cause from effect. So it is crucial to know whether vitamin D supplementation can improve erectile function. A 2018 paper by Giacomo Tirabassi and colleagues, based on a longitudinal study of 41 men seeking medical care for sexual dysfunction before and after vitamin D replacement therapy, yielded an answer. Patients repeatedly received large oral doses until the blood level of 25-hydroxyvitamin D3 reached 30 ng/mL, taking between 9 and 12 months. Increases in circulating vitamin D and improvement in erectile function were significantly positively correlated.
Concluding comments
Erectile dysfunction is surprisingly common across human populations. This is presumably yet another “disease of civilization," absent in our hunting-and-gathering ancestors. In today’s world, ED surely decreases male fertility. In a 2017 report on a study at Cairo University Hospital, Amir Gabr and colleagues compared 200 infertile couples with 200 normally fertile couples. Men in infertile couples had significantly lower scores on a scale for erectile function. Much has been written about the abrupt mid-life loss of fertility in women (menopause), and it is often implied that men have no counterpart. However, men do show a more gradual age-related decline in testosterone levels and sperm production called andropause (or, jokingly, manopause). Mainly because of hardened arteries, erectile dysfunction is an additional age-related development that can significantly reduce fertility in older men.
References
Adams, M.R., Kaplan, J.R., Koritnik, D.R., Weaver, D.S. & Bond, M.G. (1984) Erectile failure in cynomolgus monkeys with atherosclerosis of the arteries supplying the penis. Journal of Urology 131:571-573.
Aytaç, I.A., McKinlay, J.B. & Krane, R.J. (1999) The likely worldwide increase in erectile dysfunction between 1995 and 2025 and some possible policy consequences. BJU International 84:50-56.
Barassi, A., Pezzilli, R., Colpi, G.M., Corsi Romanelli, M.M. & Melzi d'Eril, G.V. (2014) Vitamin D and erectile dysfunction. Journal of Sexual Medicine 11:2792-2800.
Christ, G.J., Andersson, K.E., Williams, K., Zhao, W., D’Agostino, R., Kaplan, J., Aboushwareb, T., Yoo, J., Calenda ,G., Davies, K.P., Sellers, R.S. & Melman, A. (2009) Smooth-muscle-specific gene transfer with the human maxi-K channel improves erectile function and enhances sexual behavior in atherosclerotic cynomolgus monkeys. European Urology 56:1055-1066.
Dumbraveanu, I., Banov, P., Arian, I. & Ceban, E. (2020) The correlations of clinical and biochemical indices of vitamin D with erectile dysfunction. Journal of Medicine & Life 13:144-150.
Farag, Y.M.K., Guallar, E., Zhao, D., Kalyani, R.R., Blaha, M.J., Feldman, D.I., Martin, S.S., Lutsey, P.L., Billups, K.L. & Michos, E.D. (2016) Vitamin D deficiency is independently associated with greater prevalence of erectile dysfunction: The National Health and Nutrition Examination Survey (NHANES) 2001-2004. Atherosclerosis 252:61-67.
Gabr, A.A., Omran, E.F., Abdallah, A.A., Kolb, M.M., Farid, E.Z., Dieb, A.S. & Belal, D.S. (2017) Prevalence of sexual dysfunction in infertile versus fertile couples. European Journal of Obstetrics & Gynecology and Reproductive Biology 217:38-43.
Kessler, A., Sollie, S., Challacombe, B., Briggs, K. & Van Hemelrijck, M. (2019) The global prevalence of erectile dysfunction: a review. BJU International 124:587-599.
Lombardi, G., Nelli, F., Celso, M., Mencarini, M. & Del Popolo, G. (2012) Treating erectile dysfunction and central neurological diseases with oral phosphodiesterase type 5 inhibitors: Review of the literature. Journal of Sexual Medicine 9:970-985.
Tirabassi, G., Sudano, M., Salvio, G., Cutini, M., Muscogiuri, G., Corona, G. & Balercia, G. (2018) Vitamin D and male sexual function: A transversal and longitudinal study. International Journal of Endocrinology 2018,3720813:1-8.
Weingand, K.W. (1989) Atherosclerosis research in cynomolgus monkeys (Macaca fascicularis). Experimental & Molecular Pathology 50:1-15.
Williams, J.K., Andersson, K.-E. & Christ, G. (2012) Animal models of erectile dysfunction (ED): Potential utility of non-human primates as a model of atherosclerosis-induced vascular ED. International Journal of Impotence Research 24:91-100.




