Health
Antibiotic Apocalypse: Going, Going, Gonorrhoea
Some superbugs may be winning the arms race against antibiotics.
Posted October 29, 2019
The discovery of antibiotics was a huge medical breakthrough that saved countless lives around the world. Unfortunately, many harmful bacteria have become immune to antibiotics through adaptation under selection, a process that underlies all evolutionary change. Several “superbugs” resistant to multiple antibiotics have now emerged.
Change under selection is inevitable, but squandering antibiotics has worsened matters. Imprudent use to treat human infections is often seen as the main culprit. But the main factor is the immoderate application of antibiotics in animal husbandry, largely to promote growth and boost profits rather than to treat infections. In some countries, farming is responsible for 80% of antibiotic resistance! Because lower-income countries are misusing antibiotics ever more widely in agriculture, unchecked global usage could triple by 2030. In 2013, the Centers for Disease Control and Prevention (CDC) estimated that in the USA over two million people contract antibiotic-resistant infections every year, with fatal results for at least 23,000. CDC’s Director, Tom Frieden, recently warned of an impending “post-antibiotic era". The World Health Organization (WHO) has acted to promote international awareness and concerted action, notably to curb agricultural use.
Natural selection — the Darwin/Wallace breakthrough
Independent discoveries led Darwin and Wallace to conclude that all organisms change over time, and Darwin’s 1859 book title aptly emphasized the fundamental mechanism: he name it On the Origin of Species by Means of Natural Selection in the Struggle for Life. Doubters often dismiss evolution as “just a theory,” but natural selection is not a conjecture. The genius of Darwin and Wallace resided in their insight that natural selection is inevitable and universal. On the first encounter with the theory, British biologist Thomas Huxley commented: “How stupid not to have thought of that.”
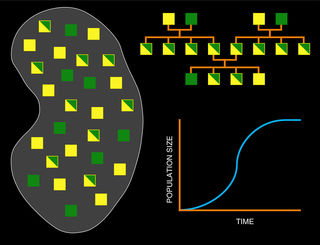
Natural selection has three basic components: First, populations generally produce more offspring than can survive, so substantial mortality is inevitable. Second, many features show inherited variation. Third, in any given environment certain hereditary variants enhance survival while others reduce it. That’s all it needs. A simple computer program with those components automatically generates cumulative change. It is like a mathematical equation: Excess offspring + inherited variation + survival differences = evolution.
Bacteria, antibiotics, selection
Following Darwin and Wallace, biologists have discovered and studied many cases of evolution in action. A particularly striking example poses a major threat to human health: drug-resistant bacteria. Human ingenuity gave us antibiotics such as penicillin, which generates a toxic environment for bacteria. The ideal outcome would be to eliminate all hostile bacteria in one rapid sweep. But human bodies, particularly our guts, also house beneficial bacteria. So aggressive antibiotics or large doses can have serious side-effects. Medical remedies are designed to kill the disease without killing the patient. This tempered approach permits hostile bacteria bearing mutations that shield them against antibiotics to survive and multiply.
Antibiotics thus promote the breeding of resistant mutants, which rapidly increase in numbers. Resistance develops in two main ways, either through the production of new enzymes that destroy antibiotics or through structural changes that shield the bacterial surface from recognition. Eventually, any antibiotic will become ineffective. Unintended selection thrusts medical science into an arms race in which the success of any new antibiotic is steadily eroded by steadily spreading resistance.
Of course, drug-resistant bacteria are not products of natural selection because antibiotics are artificial. But the mechanism is just the same. Bacteria divide and multiply so rapidly that they would rapidly clog the planet if not held in check. Inherited variability fed by mutation is present in bacteria just as in all other living things. And antibiotics serve as selective agencies, favoring particular genetic variants and drastically limiting propagation of all others.
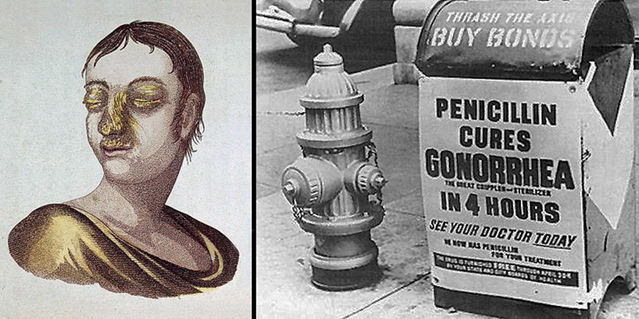
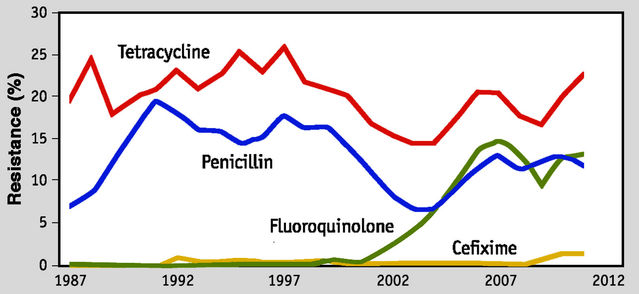
The example of gonorrhea
Resistance is also posing increasing problems with sexually transmitted diseases (STDs) such as chlamydia, gonorrhea, and syphilis, which are treated with antibiotics. In fact, curing syphilis has long been a prevalent use of penicillin. The 2 million people infected with difficult-to-treat STDs in the USA every year include an increasing number of cases of antibiotic-resistant gonorrhea. This disease has become exceedingly difficult to treat and counts among three “urgent threats” that the CDC identified in 2013. Many antibiotics once used to treat gonorrhea have gradually become ineffective and the last remaining line of treatment requires two potent antibiotics: azithromycin combined with ceftriaxone.
In recent years, increasing resistance has been encountered with azithromycin, and a few cases of resistance to ceftriaxone have just been reported in Hawaii. Syphilis and chlamydia give less cause for concern as yet but have also begun to show antibiotic resistance in some regions. It is only a matter of time before treatment-resistant cases begin to surface.
Universal occurrence of resistant strains of bacteria is now a major health threat to any patient admitted to a hospital, especially for surgery. Regrettably, incautious usage makes matters worse. Using antibiotics for minor aliments rather than reserving them for life-threatening illness greatly increases the scope for breeding resistant strains of bacteria. It is also counter-productive for patients to take antibiotics irregularly or stop taking them before they have had time to work properly. For some time, I assumed that the wasteful use of antibiotics in treating human infections was the primary driver of antibiotic resistance. But abundant evidence has revealed that the predominant cause of this rampant problem is the administration of antibiotics to farm animals.
Antibiotic Apocalypse is nigh
The 2013 CDC report described antibiotic resistance as “one of the biggest public health challenges of our time”. It provided a comprehensive review of 18 leading threats from antibiotic resistance in the USA. The authors estimated that gonorrhea cases in the USA total 820,000 per year. Of these, fewer than 1% fail to respond to the currently recommended double-antibiotic treatment. But resistance to older, less expensive antibiotics is far higher, pointing to future problems.
More recently, a 2018 paper by Eili Klein and colleagues reviewed global trends in antibiotic consumption between 2000 and 2015 across 76 countries. Over that 15-year period, consumption increased by 65%, driven mainly by low- and middle-income countries as their economies grew. Although rates of antibiotic consumption in low-income countries were generally lower, they were rapidly approaching those in high-income countries. Klein and colleagues calculated that, if no policy changes occurred, by 2030 global antibiotic consumption would triple. Across the board, surging use of last-resort antibiotics was a particular cause of concern.
Mounting resistance has led to the emergence of super-bugs resistant to multiple antibiotics. The six most prevalent bacteria of this kind are grouped together under the acronym ESKAPE: Enterococcus, Staphylococcus, Klebsiella, Acinetobacter, Pseudomonas, Enterobacter. In 2018, the Paris-based Organization for Economic Cooperation and Development published a report entitled Stemming the Superbug Tide: Just A Few Dollars More. Combining several advanced techniques, OECD analyzed available information to provide a basis for policy action. Several cost-effective initiatives to combat resistance were proposed, notably more prudent use of antibiotics, improved prevention of infection and increased deployment of vaccinations.
Count-down to Armageddon
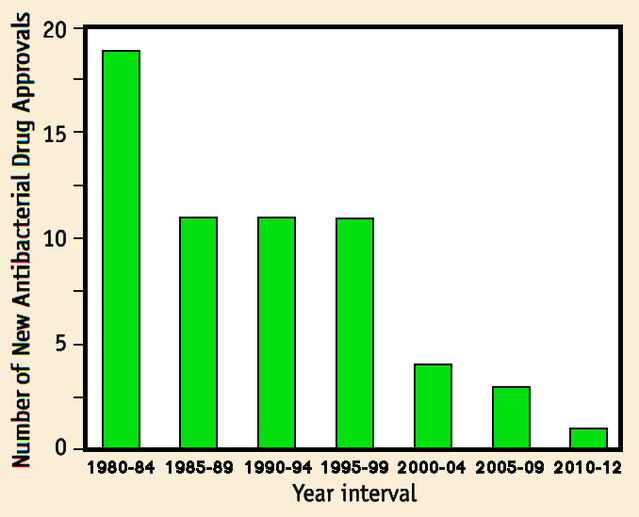
Urgent international action could forestall the gathering crisis caused by rising antibiotic resistance, but several obstacles must first be overcome. One might expect that, as in the past, the discovery of new kinds of antibiotics could come to the rescue. However, the rate of introduction of new antibiotics has steadily declined over the past 20 years. A major factor is that research and development costs are extremely high whereas financial returns are relatively low. So the drug pipeline does not have much to offer right now. We also face the problem that antibiotic usage is expanding rapidly around the globe, with animal husbandry continuing to outpace medical applications by a wide margin. The international community must heed warnings from the World Health Organization and implement a comprehensive strategy to constrain the current misuse of antibiotics to buy time while alternative tactics are explored.
Last but not least, this one case alone quite clearly shows why instruction about the universal action of selection on living things — evolutionary biology — should be a mandatory part of any secondary school syllabus.
References
CDC (2013) Antibiotic Resistance Threats in the United States, 2013. Atlanta, GA: Centers for Disease Control & Prevention.
See also:
https://www.cdc.gov/drugresistance/index.html
Klein, E.Y., Van Boeckel, T.P., Martinez, E.M., Pant, S., Gandra, S., Levin, S.A., Goossens, H. & Laxminarayan, R. (2018) Global increase and geographic convergence in antibiotic consumption between 2000 and 2015. Proceedings of the National Academy of Sciences U.S.A. 115: E3463-E3470.
Organization for Economic Cooperation and Development (2018) Stemming the Superbug Tide: Just A Few Dollars More. Paris: OECD Publishing.
Qin, L., Wang, J., Lu, J., Yang, H., Zheng, R., Liu, Z., Huang, X., Feng, Y., Hu. Z. & Ge, B. (2019) A deletion in the RD105 region confers resistance to multiple drugs in Mycobacterium tuberculosis. BMC Biology 17,7:1-12.
Sánchez-Busó, L., Golparian, D., Corander, J., Grad, Y.H., Ohnishi, M., Flemming, R., Parkhill, J., Bentley, S.D., Unemo, M. & Harris, S.R. (2019) The impact of antimicrobials on gonococcal evolution. Nature Microbiology 4:1-10.
Terra, L., Dyson, P.J., Thomas, L., Abdelhameed, A., Banat, I.M., Gazze, S.A., Vujaklija, D., Facey, P.D., Francis, L.W. & Quinn, G.A. (2018) A novel alkaliphilic Streptomyces inhibits ESKAPE pathogens. Frontiers in Microbiology 9,2458:1-1.
Van Boeckel, T.P., Pires, J., Silvester, R., Zhao, C., Song, J., Criscuolo, N.G., Gilbert, M., Bonhoeffer,S. & Laxminarayan, R. (2019) Global trends in antimicrobial resistance in animals in low- and middle-income countries. Science eaaw1944:1-5.
Walsh, C. (2000) Molecular mechanisms that confer antibacterial drug resistance. Nature 406:775-781.
WebMD Medical Reference (2019) Antibiotic-Resistant STDs: FAQ
https://www.webmd.com/sexual-conditions/antibiotic-resistant-std-faq
World Health Organisation (2011) Emergence of multi-drug resistant Neisseria gonorrhoeae – Threat of global rise in untreatable sexually transmitted infections. Geneva, Switzerland: World Health Organisation.




