Depression
Tackling Treatment Resistant Depression with Multiple Tools
Ketamine changed lives and opened minds, but it's no panacea.
Posted May 6, 2024 Reviewed by Kaja Perina
Key points
- Ketamine changed lives and opened minds to alternative treatments for mental health.
- Yet Ketamine is no panacea for treatment-resistant depression and other debilitating mental health conditions.
- Other solutions exist that are helping to make treatment-resistant conditions more treatable than ever before.
After administering more than 23,000 ketamine treatments over the past 5 years, we obviously believe in the drug’s importance—saving and changing lives of many patients who suffer from intractable mental health disease.
.png.jpg?itok=RwuuG0-x)
But ketamine is no panacea for treatment-resistant depression (TRD) and other debilitating mental health conditions. Other solutions exist that are helping to make treatment-resistant conditions more treatable than ever before. And while the explosion of ketamine-for-cash clinics did a lot to build awareness of ketamine, it also provided a myopic, wonder-drug view that overlooks alternatives.
In this blog, we will provide a quick overview of a few key treatments that are helping to make the term treatment-resistant somewhat archaic. We will omit treatments that are currently illegal or require hospitalization.
TMS–a non-drug, non-invasive alternative
Transcranial magnetic stimulation has long been a mainstay of our mental health practice. It’s been a completely noninvasive, non-drug, FDA-approved treatment for depression and OCD for nearly 15 years. According to a study published by the Journal of Neuropsychiatry, “Response to [TMS] treatment is variable, with response rates reported between 45% and 60% and remission rates between 30% and 40%.”

Why we choose this alternative: When a patient is treatment-resistant, having failed at least two traditional antidepressants, we often try TMS rather than continue to trial additional antidepressant medications. TMS is an important treatment for patients needing to avoid medications due to pregnancy or side effects.
Over the years, the technology and research behind TMS has steadily improved. Recently, researchers found that one of the many impacts TMS has on the brain is to correct the flow of brain signals. Researchers at Stanford Medicine studied 33 individuals with major depressive disorder and found that their brain signals were traveling in the wrong direction. After treating the participants with TMS, the flow of neural activity reversed directions and resulted in a lift in mood.
While not everyone with depression has an abnormal flow of neural activity, this is one possible cause of depression. In fact, we often begin our treatment intervention with TMS because it is well tolerated with minimal side effects and non-invasive.
Vagal Nerve Stimulation–an implantable option
Vagal Nerve Stimulation (VNS) is an FDA-approved, non-medication treatment option for severe or bipolar depression. Like ketamine, it has a 70% success rate when used for TRD, meaning the patient hasn’t responded to traditional antidepressants.
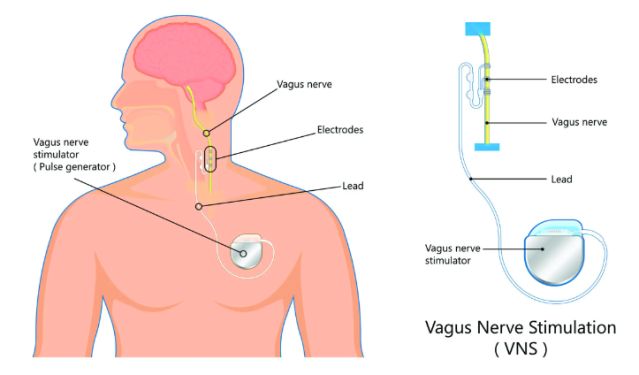
Vagus Nerve Stimulation for depression involves implanting a small device just below the skin in the upper chest, similar to a pacemaker. VNS stimulates the vagus nerve, triggering its natural process of sending electrical pulses to parts of the brain that control mood.
Why we use this alternative: One thing to note is that VNS is considered an adjunct treatment, meaning it is typically used in tandem with an antidepressant or other treatment. We believe VNS could be the ‘ketamine reduction’ device providing a safe, enduring treatment beyond medication options. It gives mental health patients another vital option that works with your body’s natural means of controlling mood.
VNS is a proven treatment that has been around for more than 25 years and has been used in over 130,000 people. With recent advancements in the VNS technology and implantable devices, it has become much more accessible to the patients who need it most.
A small 2022 study of TRD patients in China found that, after 9 months of treatment with VNS, the response and remission were 85.7% and 57.1%, respectively. Meanwhile, a much larger clinical trial is underway since 2019 and will run until 2028 to “determine whether active VNS Therapy treatment is superior to a no stimulation control in producing a reduction in baseline depressive symptom severity.”
Though VNS is not as fast acting as most other antidepressant treatments, it can be used safely in combination with transcranial magnetic stimulation (TMS), electroconvulsive therapy (ECT), and common antidepressant medications to provide patients an added boost to break through their symptoms.
Dextromethorphan/bupropion–a (not so new) drug alternative
A new oral antidepressant, Auvelity, was approved by the FDA in 2022 following a phase 3 clinical trial study titled: Efficacy and Safety of AXS-05 (Dextromethorphan-Bupropion) in Patients With Major Depressive Disorder. According to clinical trial data, MDD patients treated with dextromethorphan-bupropion showed significant improvements in depressive symptoms compared to a placebo:
“Remission was achieved by 39.5% of patients with dextromethorphan-bupropion versus 17.3% with placebo (treatment difference, 22.2; 95% CI, 11.7 to 32.7; P < .001), and clinical response by 54.0% versus 34.0%, respectively (treatment difference, 20.0%; 95% CI, 8.4%, 31.6%; P < .001), at week 6.”
The drug is a combination of dextromethorphan (the active ingredient in Robitussin) and Wellbutrin (bupropion), an antidepressant. This was an important development that substantiated what was believed for some time; namely that dextromethorphan may have an impact on mood by affecting similar receptors to ketamine, working differently than other antidepressants.
As with ketamine, the generic ingredients can be just as powerful and more affordable. In fact, we may combine generic dextromethorphan with alternative antidepressants if a patient doesn’t tolerate Wellbutrin due to side effects or allergies.
Why we use this alternative: Ketamine must be administered in a clinic setting, due to its short-lived hallucinogenic effects and the potential for abuse. Dextromethorphan, on the other hand can be prescribed, along with an antidepressant, as an at-home regimen for patients.
We should note that the trial did not include TRD and risk of suicide among its criteria for patient selection. This is called out in an editorial by Alan F. Schatzberg, M.D. in The American Journal of Psychiatry which cautioned that early enthusiasm over Dextromethorphan/bupropion “needs to be tempered until further clinical experience is gained and more studies in patients with treatment-resistant depression are accomplished.” And Psychiatry News said, “An Axsome-sponsored trial conducted solely in patients with treatment-resistant depression failed to detect a difference between Auvelity and placebo after six weeks.”
So with the jury still out, we’re happy (if not enthusiastic) to see promising results from some of our own TRD patients with dextromethorphan as an antidepressant adjunct treatment.
Conclusion
Although ketamine and esketamine have certainly changed lives and opened minds to alternative treatments for mental health. With a number of other advancements, we hope that the term treatment-resistant becomes a thing of the past.
References
Iosifescu DV, Jones A, O’Gorman C, et al. Efficacy and safety of AXS-05 (dextromethorphan-bupropion) in patients with major depressive disorder: a phase 3 randomized clinical trial (GEMINI). J Clin Psychiatry. 2022;83(4):21m14345.
Nina Bai, Researchers treat depression by reversing brain signals traveling the wrong way. Stanford Medicine News Center. Retrieved May 15, 2023, from: https://med.stanford.edu/news/all-news/2023/05/depression-reverse-brain…
Zhang X, Qing MJ, Rao YH, Guo YM. Adjunctive Vagus Nerve Stimulation for Treatment-Resistant Depression: a Quantitative Analysis. Psychiatr Q. 2020 Sep;91(3):669-679. doi: 10.1007/s11126-020-09726-5. PMID: 32144640.
Zhang X, Guo YM, Ning YP, Cao LP, Rao YH, Sun JQ, Qing MJ, Zheng W. Adjunctive vagus nerve stimulation for treatment-resistant depression: a preliminary study. Int J Psychiatry Clin Pract. 2022 Nov;26(4):337-342. doi: 10.1080/13651501.2021.2019789. Epub 2022 Jan 13. PMID: 35023429.
Schatzberg, M.D., Alan F. Understanding the Efficacy and Mechanism of Action of a Dextromethorphan-Bupropion Combination: Where Does It Fit in the NMDA Versus mu-Opioid Story? American Journal of Psychiatry. Jul 2022 Retrieved April 17, from: https://doi.org/10.1176/appi.ajp.20220434
Kelly MS, Oliveira-Maia AJ, Bernstein M, Stern AP, Press DZ, Pascual-Leone A, Boes AD. Initial Response to Transcranial Magnetic Stimulation Treatment for Depression Predicts Subsequent Response. J Neuropsychiatry Clin Neurosci. 2017 Spring;29(2):179-182. doi: 10.1176/appi.neuropsych.16100181. Epub 2016 Nov 30. PMID: 27899052; PMCID: PMC5592731.




