From hoarding to handwashing to forever checking the stove, obsessive-compulsive disorder (OCD) takes many forms. It is an anxiety disorder that traps people in repetitive thoughts and behavioral rituals that can be completely disabling.
About 2 percent of the population suffers from OCD, according to the National Institute of Mental Health—that's more than those who experience other mental illnesses like schizophrenia, bipolar disorder, and panic disorder. OCD might begin in childhood, but it most often manifests during adolescence or early adulthood. Scientists believe that both a neurobiological predisposition and environmental factors jointly cause the unwanted, intrusive thoughts and the compulsive behavior patterns that appease those unwanted thoughts.
The disorder tends to be chronic—lasting for years, even decades—although the severity of the symptoms may wax and wane over the years. Both pharmacological and behavioral approaches—particularly Exposure and Response Prevention—have proven to be effective treatments that allow people with OCD to lead happy and fulfilling lives.
For more on causes, symptoms and treatments, see our Diagnosis Dictionary.

The first symptoms of OCD are obsessions—the unwanted ideas or impulses that occur over and over again and are meant to drive out fears, often of harm or contamination. "I will contract a deadly disease” or “My family will be harmed.”
Compulsions appear after that—repetitive behaviors such as handwashing, lock-checking, and hoarding. Such behaviors are intended to mitigate fear and reduce the threat of harm. But the effect does not last and the unwanted thoughts soon intrude all over again. People suffering from obsessive-compulsive habits may also contend with motor tics or repetitive movements, such as grimacing and jerking.
Sufferers may understand the uselessness of their obsessions and compulsions, but that is no protection against them. OCD can become so severe that it interferes with their work or relationships, or even keep them from leaving their home.
Obsessions and compulsions are the two central features of OCD, according to the DSM-5. Obsessions are persistent unwanted thoughts, urges, or images that cause distress and that individual tries to suppress or counteract. Compulsions are repetitive behaviors or mental acts that the individual performs in response to an obsession, with the goal of neutralizing the threat or alleviating distress. In addition, obsessions or compulsions must impair an aspect of daily functioning, be fairly time-consuming, and not be due to another mental health condition or substance use for a diagnosis.
A common misconception is that compulsions must be physical, such as trying out every seat on the train or touching your toes 20 times. But compulsions can also be performed mentally, such as repeating words or phrases, making mental lists of items, or continuously praying. Mental compulsions in OCD are just as distressing as physical compulsions. However, mental compulsions are by nature more hidden, so people who experience them may evade detection and go longer without finding help.
The obsessions and compulsions that characterize OCD can center around different themes. Five common categories of obsessions include:
1. Fear of contamination (germs, viruses)
2. Fear of harm (unlocked doors, electrical outlets catching fire)
3. Excessive concern with order or symmetry (even picture frames, general neatness)
4. Obsessions with the body or physical symptoms (breathing, swallowing)
5. Unwanted, intrusive thoughts (going to hell, harming family members)
People suffering from OCD therefore carry out compulsions such as washing hands or checking locks because they believe those actions will stop those bad outcomes from happening.
People often say that they’re “so OCD,” as a sign of their preference for cleanliness, order, or perfection. But there are key differences, and the two shouldn’t be conflated. The essential distinction is that OCD becomes a disorder when symptoms interfere or impair a person’s ability to function socially, professionally, or academically.
For example, someone with OCD might be chronically late for work, and maybe fired, if compulsions prevent them from leaving the house. In a family context, someone with OCD may avoid being home alone with their children, for fear that they will suddenly harm or kill their children.

OCD likely results from a confluence of factors—a biological predisposition, environmental factors including experiences and attitudes acquired in childhood, and faulty thought patterns.
The fact that many OCD patients respond to SSRI antidepressants suggests the involvement of dysfunction in the serotonin neurotransmitter system. Ongoing research suggests there may be a defect in other chemical messenger systems in the brain.
OCD may coexist with depression, eating disorders, or attention-deficit/hyperactivity disorder, and it may be related to disorders such as Tourette's syndrome, and hypochondria, though the nature of the overlap is the subject of debate.
The beginning of obsessions and compulsions in OCD can often be traced to a stressful event or life change that led to greater responsibilities, such as a new job, the birth of a child, or even puberty. These events can inflate the person’s sense of responsibility, generating anxiety and a desire to ensure that they don’t let themselves and others down by allowing bad things to happen. Case studies show that compulsions sometimes disappear in a hospital or lab setting, as the patient feels the burden of responsibility has been transferred to others.
One region thought to play a role in OCD is the basal ganglia, a collection of structures underneath the cortex that help coordinate movement; when the basal ganglia malfunctions, unwanted, involuntary movements can result.
In addition to the motor cortex, the basal ganglia also communicates with the prefrontal cortex, which is involved in planning, thinking, and awareness, so the basal ganglia may play a part in facilitating wanted thoughts and stopping unwanted thoughts. As evidence for this idea, brain activity in the cortex and basal ganglia is different in OCD and typical individuals, and stimulating part of the basal ganglia can reduce symptoms of OCD.
Infection sometimes plays a role in psychiatric illnesses, and research suggests that rare cases of OCD can be traced back to complications from an infection of strep throat. Psychiatric symptoms resulted after the infection, perhaps triggered by the child’s immune response, such as intrusive thoughts or impulses and the inability to abandon compulsive behaviors. This suggests that this rare route for OCD is transmissible.
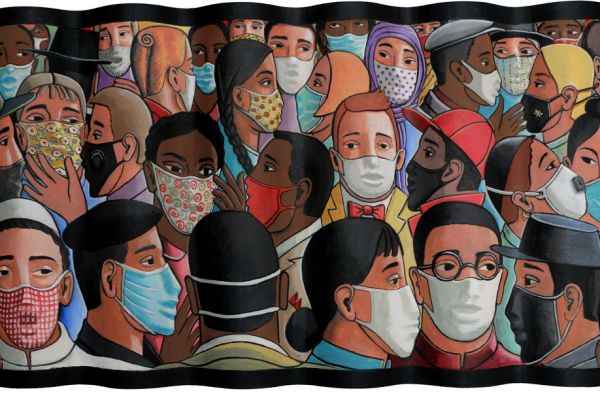
It’s possible that the pandemic may have triggered OCD for some already predisposed, but overall COVID-19 has not created an “epidemic of OCD.” A key distinction is that the fear of contracting or transmitting COVID-19 is genuine cause for concern, whereas the intrusive thoughts characteristic of the disorder are not. In most cases, extra hand-washing and sanitizing also hasn’t led to impairment or dysfunction in daily life. By contrast, someone with OCD might begin to wash their hands so many times that they become raw or bloody.

Either psychotherapy or medication, or both, may be prescribed for OCD, and research suggests that a combination of the two is often the most successful approach, especially for young people.
These drugs are typically selective serotonin reuptake inhibitors (SSRI). The SSRIs fluoxetine (Prozac), fluvoxamine (Luvox), and paroxetine (Paxil) have been specifically approved to treat OCD. These drugs have been shown to reduce the frequency and severity of obsessions and compulsions in more than half of patients, although discontinuation of drugs often leads to relapse.
Behavioral therapy for OCD such as Exposure and Response Prevention tends to produce long-lasting effects. Psychotherapy generally focuses on two aspects of the disorder: unraveling the irrational thoughts involved in the condition and gradually exposing sufferers to the feared object or idea until they are desensitized to it and can tolerate anxiety without engaging in compulsive rituals.
If a loved one is suffering from OCD, there are a few important steps to take—and a few important steps to avoid. Do not help the person carry out compulsions even if it seems reassuring, and do not tell them to “just stop it” or suggest that they’re lazy or lack willpower—these are a few of the myths about OCD. Instead, research the condition and recognize that OCD is treatable with therapy and medication, and there are secondary options if the first attempt at treatment isn’t effective. You can then gently but firmly begin a discussion about seeking help.
Exposure and Response Prevention (ERP) is a frontline treatment for OCD. ERP is a form of cognitive behavioral therapy, and it involves safely exposing the patient to the feared stimuli (exposure) and preventing the typical ritual they would perform in response (response prevention).
For example, if a patient has obsessions about contamination leading him to contract a deadly illness, the therapist might help him touch a sink, door handle, or floor, and then have him eat lunch without being allowed to wash his hands. Although this is anxiety-inducing at first, it helps the patient learn that their fear will not materialize.
Two models propose why ERP is effective. The habituation model proposes that getting used to the feared stimulus changes behaviors, which in turn changes beliefs, which in turn alters the emotions involved. The inhibitory learning model suggests that the connection hasn’t been broken, but that patients develop cognitive and emotional flexibility around what the outcome can be in the presence of the feared stimulus.
Simply trying to suppress distressing thoughts doesn’t work. In a well-known experiment, psychologist Daniel Wegner asked study participants not to think about white bears—and naturally white bears were all they could think about.
Instead, a few cognitive techniques can help to overcome obsessive thoughts in OCD. One is to prove that thoughts don’t control reality by exposing yourself (or your thoughts) to your fear, which is a component of exposure therapy for OCD. Exposure and Response Prevention. Another is to “float” your obsession; instead of trying to get rid of it, envision it floating down a river and becoming smaller as you focus on your breathing.
Early diagnosis and treatment can, in some cases, lead to a full recovery. While obsessions and compulsions do not completely disappear for many others, treatment still allows them to lead a fulfilling life. And having realistic expectations for recovery can help; people who expect to fully abolish their OCD may be disappointed with their clinician, themselves, and life. But people who have the expectation that “OCD will occupy a smaller part of my life” or that “It will bother me sometimes, but I’ll have the skills to handle it” set themselves up to be happier and more satisfied.
Like all other aspects of life, the pandemic has upended treatment for OCD, because Exposure and Response Prevention, the gold-standard of treatment, is an interactive and hands-on form of therapy. As a result, therapists have shifted their approach. They may have changed patients’ exposure plans based on which actions are due to the pandemic and which are not, focused on how the patient is spending their time to avoid expanding the time allotted to obsessions and compulsions, and explored prescribing medication when appropriate.
A lapse in OCD, the brief or partial return of symptoms like compulsive behaviors, can be due to stress, life transitions, or new environments that evoke an obsession. But lapses don’t have to lead to a full relapse. To avoid relapses, people can identify what triggered the setback and develop a plan to navigate that situation in the future. Continuing to practice CBT and/or ERP is key to maintaining recovery as well.